JAHA:心律失常性心肌病患者左室功能障碍的临床意义
2021-04-06 MedSci原创 MedSci原创
AC患者首次就诊时,更多的运动暴露与LV功能恶化相关,但在随访期间对LV进展没有显著影响。LV功能障碍的进展最明显的是去纤维血小板溶素基因型患者。
心律失常性心肌病(AC)的特征是双心室功能障碍、不耐受运动、室性心动过速和猝死高风险。左室(LV)疾病的易感因素及其预后意义在AC患者中很少进行归纳。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在评估运动暴露和基因型与AC患者左室功能障碍之间的相关性,并探讨LV疾病进展对不良心律失常结局的影响。
在这项纵向研究中,研究人员纳入了168例AC患者(50%先证者,45%女性,40±16岁),共接受了715次超声心动图检查(4.1±1.7次/例,随访7.6次[四分位数范围(IQR)为5.4-10.9]年),并获得了完整的运动和遗传数据。
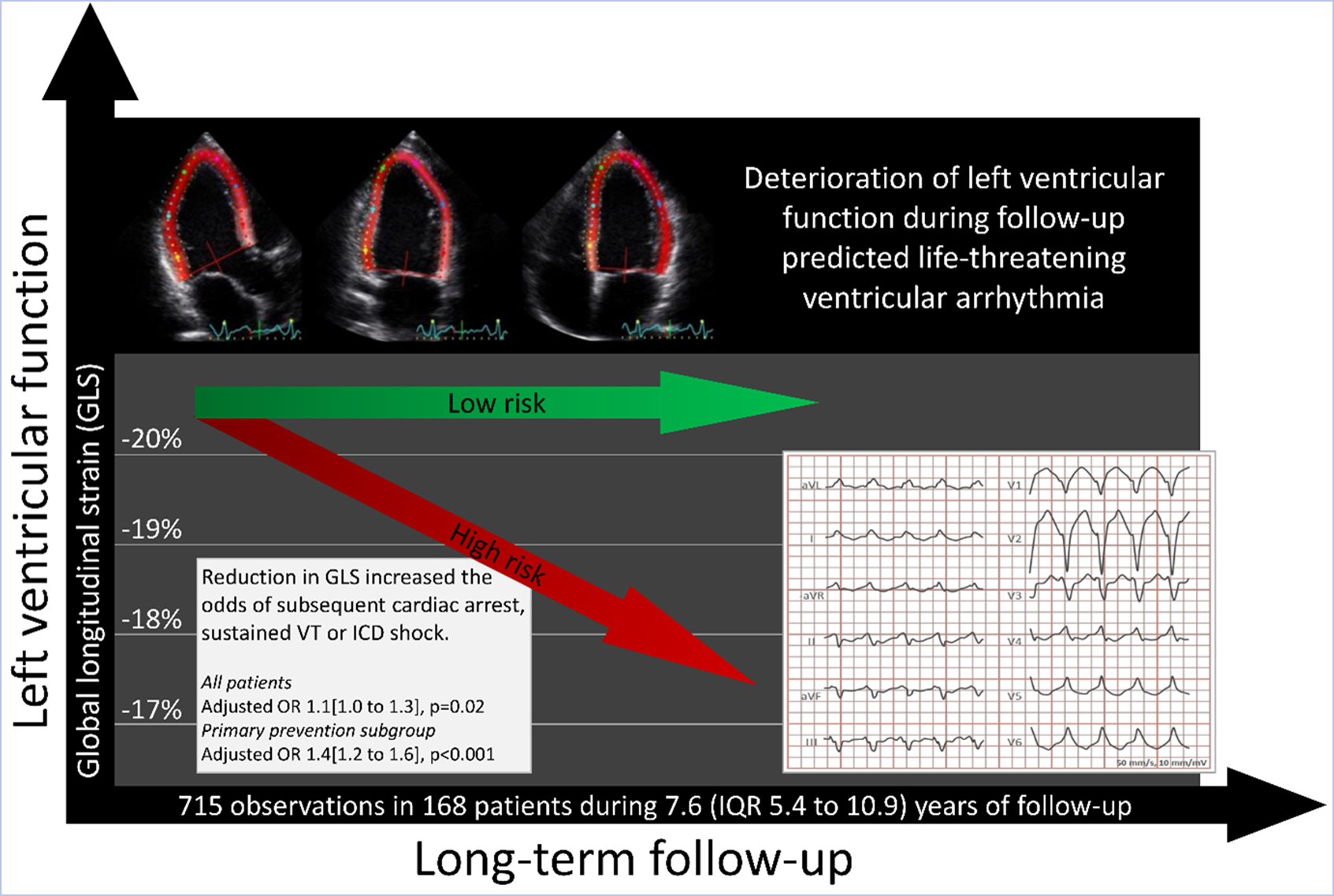
患者就诊时,通过整体纵向应变反映的左室功能为-18.8% [IQR为-19.2%至-18.3%],而在运动暴露程度较高的患者中,左室功能更差(整体纵向应变恶化,0.09% [IQR为0.01%-0.17%]/5 MET‐小时/周,P=0.02)。整体纵向应变导致左室功能恶化,每年为0.08% [IQR为0.05%-0.12%];(P<0.001),纤维血小板溶素基因型患者中进展最为明显(相互作用P<0.001)。LV功能恶化可预测室性心动过速(心脏骤停、持续性室性心动过速、或植入式心律转复除颤器休克)(调整比值比为1.1 [IQR为1.0-1.3]/整体纵向应变恶化1%;P=0.02,调整时间和之前的心律失常事件)。
由此可见,AC患者首次就诊时,更多的运动暴露与LV功能恶化相关,但在随访期间对LV进展没有显著影响。LV功能障碍的进展最明显的是去纤维血小板溶素基因型患者。随访期间LV功能恶化可预测随后的室性心动过速,并应将其纳入风险分层。
原始出处:
Øyvind H. Lie.et al.Left Ventricular Dysfunction in Arrhythmogenic Cardiomyopathy: Association With Exercise Exposure, Genetic Basis, and Prognosis.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.018680
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#左室功能#
46
好文
65
#心律失常性心肌病#
59
#AHA#
62
#功能障碍#
68
#肌病#
61
学习学习
105