Eur Heart J:既往有心脏病的COVID-19住院患者临床表现、病程和结局
2021-11-06 MedSci原创 MedSci原创
心脏病亚型与住院死亡率之间的关联强度存在相当大的异质性。在所有心脏病患者中,心衰患者因COVID-19住院的死亡风险最大。住院期间很少发生严重的心脏并发症。
自2019年12月以来,2019冠状病毒病(COVID-19)在全球迅速蔓延,截至2021年9月19日,已确诊病例超过2.25亿,死亡人数接近470万。患有心脏病的患者被认为在COVID-19住院后出现不良结果的高风险。
 近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究的目的是评估各种心脏病亚型与患者院内死亡率之间关联的异质性。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究的目的是评估各种心脏病亚型与患者院内死亡率之间关联的异质性。
研究人员使用了CAPACITY-COVID登记中心和LEOSS研究的数据,并拟合多变量泊松回归模型以评估不同类型的心脏病与患者住院死亡率之间的关联。
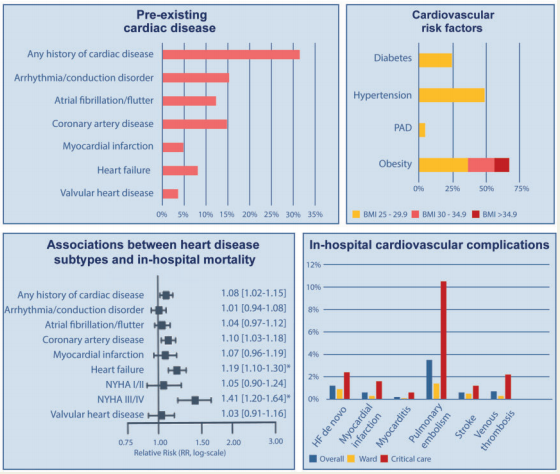
该研究共纳入了16511名COVID-19患者(21.1%的患者年龄在66-75岁;40.2%为女性),31.5%的受试者有心脏病史。伴有心脏病的患者年龄较大,主要为男性,与不伴有心脏病的患者相比,通常有其他合并症。心脏病患者的死亡率更高(29.7%;n=1545 vs. 15.9%;n=1797)。然而,经过多变量调整后,这种差异并不显著[调整后的风险比(aRR)为1.08,95%置信区间(CI)为1.02-1.15;P=0.12]。心脏病亚型与院内死亡率的相关性差异很大,与心力衰竭的相关性最强(aRR为1.19,95%CI为1.10-1.30;P<0.018),尤其是重度(纽约心脏协会III/IV级)心力衰竭(aRR为1.41,95%CI为1.20-1.64;P<0.018)。在多变量调整后,包括缺血性心脏病在内的其他心脏病亚型均不显著。1%以下的患者被诊断出严重的心脏并发症。
由此可见,心脏病亚型与住院死亡率之间的关联强度存在相当大的异质性。在所有心脏病患者中,心衰患者因COVID-19住院的死亡风险最大。住院期间很少发生严重的心脏并发症。
原始出处:
The CAPACITY-COVID Collaborative Consortium and LEOSS Study Group.et al.Clinical presentation, disease course, and outcome of COVID-19 in hospitalized patients with and without pre-existing cardiac disease: a cohort study across 18 countries.European Heart Journal.2021.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehab656/6420641
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ART#
54
#HEART#
56
很详细的讲解,谢谢
83
热点话题
89