肺动脉高压和右心室功能障碍的术后血流动力学指标与左心室辅助装置植入后临床结果的相关性
2022-08-23 刘少飞 MedSci原创
虽然左心室辅助装置(LVAD) 手术后与早期右心衰竭(RHF)相关的术前血流动力学危险因素已得到充分确立,但术后血流动力学状态与后续结果之间的关系仍不清楚。
虽然左心室辅助装置(LVAD) 手术后与早期右心衰竭(RHF)相关的术前血流动力学危险因素已得到充分确立,但术后血流动力学状态与后续结果之间的关系仍不清楚。
病人的入选:
胸外科学会机械辅助循环支持机构间登记处(STS-INTERMACS)的方案得到了美国国家卫生研究院、阿拉巴马大学伯明翰分校数据协调中心的机构审查委员会以及各参与医院的机构审查委员会的批准。本研究放弃了对知情同意的要求。
研究方法:
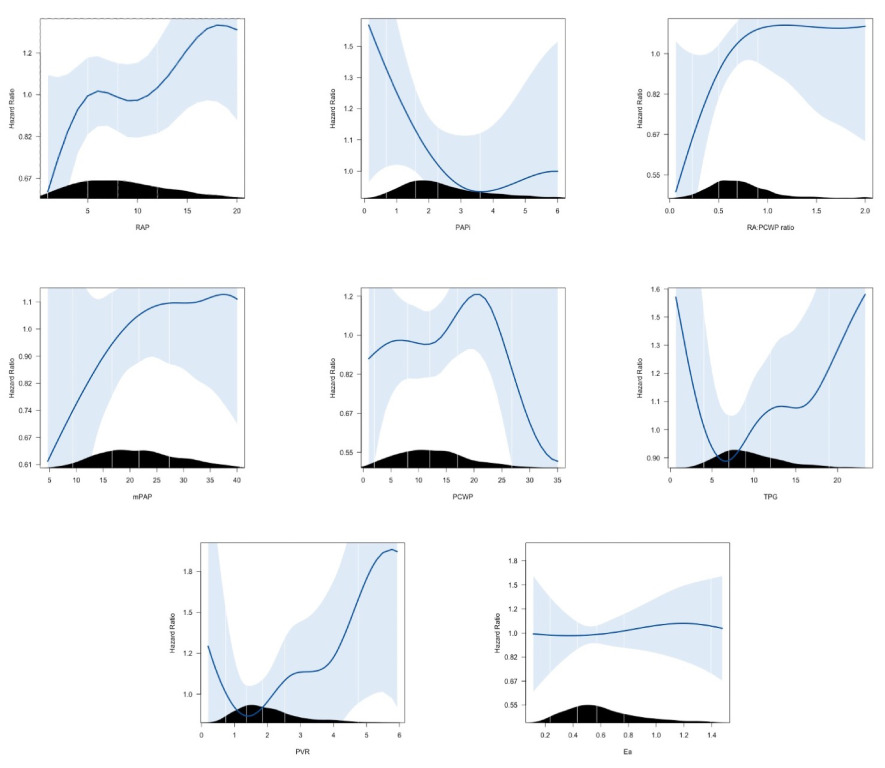
我们分析了来自 STS-INTERMACS 登记的成年 CF-LVAD 患者,这些患者在没有早期 RHF 证据的情况下存活了至少 3 个月,并且在 LVAD 植入后 3 个月可获得血流动力学数据。使用多变量 Cox 比例风险模型评估RV 后负荷和功能指标与随后的死亡、右心衰竭(RHF)、胃肠道出血(GIB) 或中风风险之间的关联。
研究结果:
在 1,050 名 3 个月血流动力学可用的患者中,肺动脉高压很常见,其中 585 名 (55.7%) 的mPAP ≥ 20 mm Hg 和 164 名 (15.6%) 的PVR ≥ 3 WU。肺动脉搏动指数(PAPi,HR 0.62/log-increas for values < 3, 95% CI 0.43-0.89)和PVR(HR 1.19 per 1 WU-increas for values > 1.5 WU, 95% CI 1.03-1.38)是独立的与死亡或 RHF 的复合相关。术后RAP (HR 1.18 每增加 5 mm Hg,95% CI 1.04-1.33),RAP:PCWP(HR 1.46 每增加对数,95% CI 1.12-1.91)和 PAPi(HR 0.76 每增加对数,95% CI 0.61-0.95)均与 GIB 风险相关。术后血流动力学与卒中风险无关。
研究结论:
在这项研究中,我们已经表明 LVAD 植入后早期 RV 功能障碍的血流动力学标志物和增加的 RV 后负荷与死亡、LRHF 和 GIB 的风险独立相关。虽然在我们的分析中确定为显着的特定血流动力学标志物因结果而异,但 PAPi 和 PVR 似乎始终与不良结果相关。术后RV 功能障碍和 RV 后负荷升高的血流动力学指标与 RHF、死亡率和 GIB 独立相关。针对RV 功能和后负荷术后优化的策略是否可以减轻这些不良事件的负担需要前瞻性研究。
参考文献:
Gulati G, Grandin EW, DeNofrio D, Upshaw JN, Vest AR, Kiernan MS. Association between postoperative hemodynamic metrics of pulmonary hypertension and right ventricular dysfunction and clinical outcomes after left ventricular assist device implantation. J Heart Lung Transplant. 2022 Jul 23:S1053-2498(22)02029-0. doi: 10.1016/j.healun.2022.07.005. Epub ahead of print. PMID: 35970648.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血流动力#
67
#左心室辅助装置#
115
#心室辅助装置#
99
#动脉高压#
104
#临床结果#
69
#相关性#
62
#右心室功能#
69
#血流动力学#
73
#左心室#
102
#功能障碍#
92