赵军医生:记多科室协作成功抢救凶险性前置胎盘产妇术中大出血并保留子宫1例
2015-01-04 赵军 新青年麻醉论坛
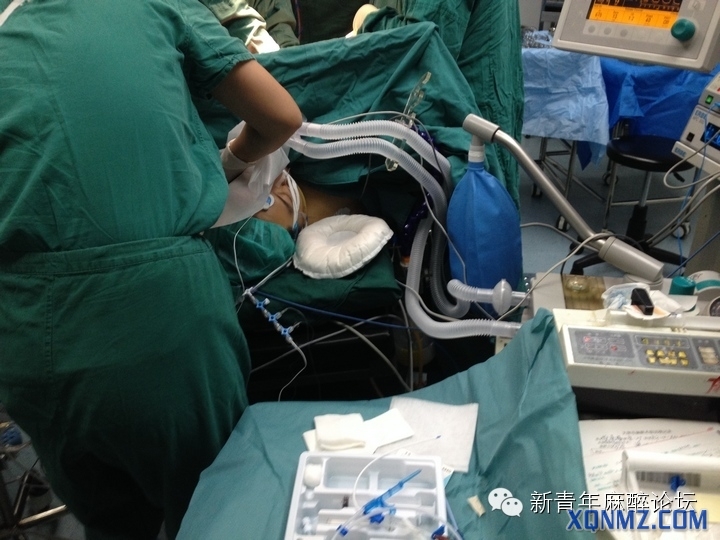
麻醉医生-----无影灯下的幕后英雄 记多科室协作成功抢救凶险性前置胎盘产妇术中大出血并保留子宫1例 导言:手术室内,麻醉医生的主要职责是为围术期患者提供全方位的安全、舒适保障,并不只是打一针这么简单。而这,也只是麻醉工作的一部分。现代医学飞速发展,作为麻醉医生,我们的路,才刚刚开始。 短短十几秒钟,失血量竞超过1000m

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








赞
167
#军医#
34
#大出血#
35
#前置胎盘#
56
#胎盘#
24
#抢救#
42