J Periodontal Res:长非编码RNA anril与牙周炎和心血管疾病的关系
2018-09-27 MedSci MedSci原创
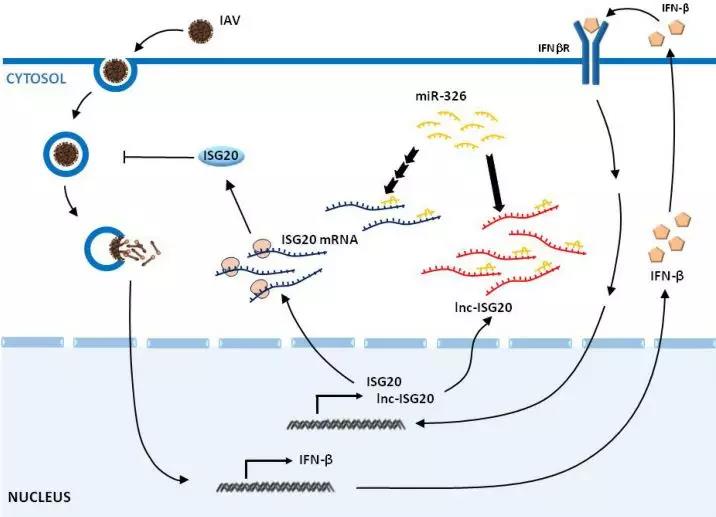
已证实重度牙周炎与心血管疾病(CVD)相关的生物学合理性。遗传特征在复杂的炎症疾病中起重要作用。长非编码RNA中的多态性(单核苷酸多态性[SNP]),INK4基因座中的反义非编码RNA(ANRIL)在两种疾病中起主导作用。该研究的主要目的是评估心血管(CV血管造影证实≥50%主冠状动脉狭窄)患者,ANRIL SNPs rs133049和rs3217992对牙周炎严重程度和既往冠状动脉病史的影响,以
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#非编码#
52
#PE#
35
#长非编码RNA#
55
#牙周#
38
#编码#
36
#血管疾病#
30
学习了长知识
53
学习了长知识
51
学习了长知识
59
学习了长知识
68