Circ Cardiovasc Inte:大隐静脉移植介入治疗中药物洗脱支架vs. 裸金属支架
2018-12-06 国际循环编辑部 国际循环
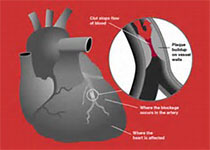
经皮冠状动脉介入治疗(PCI)中,药物洗脱支架(DES)被越来越多地用于大隐静脉移植狭窄的血运重建,但尚无有利于其使用的强有力临床证据。在大隐静脉移植行PCI的患者中,有关DES与裸金属支架(BMS)的随机对照试验尚无定论。Circulation:Cardiovascular Interventions发表的这项研究对此进行了探讨。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#洗脱支架#
63
#ASC#
75
#金属支架#
80
#静脉#
41
#大隐静脉#
71
#裸金属支架#
60
#药物洗脱支架#
78
了解一下,谢谢分享!
99