科学家发明恶性肿瘤“分子手术刀”
2015-10-28 王春儒等 科学网
如何实现精准的肿瘤靶向治疗而不损伤正常组织一直是医学界追求的目标。最近,中科院化学所王春儒团队开发的基于金属富勒烯纳米颗粒的“分子手术刀”肿瘤治疗技术,在实现这一梦想的道路上前进了一大步。 众所周知,实体肿瘤组织实际上是由肿瘤细胞和肿瘤血管形成的一个完整微环境系统,不仅包含肿瘤细胞,内部还有丰富的肿瘤血管。现代生物医学研究已经证明,肿瘤血管与正常血管在结构上存在巨

如何实现精准的肿瘤靶向治疗而不损伤正常组织一直是医学界追求的目标。最近,中科院化学所王春儒团队开发的基于金属富勒烯纳米颗粒的“分子手术刀”肿瘤治疗技术,在实现这一梦想的道路上前进了一大步。
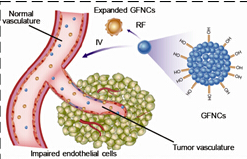
众所周知,实体肿瘤组织实际上是由肿瘤细胞和肿瘤血管形成的一个完整微环境系统,不仅包含肿瘤细胞,内部还有丰富的肿瘤血管。现代生物医学研究已经证明,肿瘤血管与正常血管在结构上存在巨大差异。一般来说,正常血管需要一年时间才能够长成,是由内膜、中膜和外膜构成的三层密实结构,而肿瘤血管只用4天即可形成,结构上为由内皮细胞构成的单层薄膜。而由于构成肿瘤血管的内皮细胞间隙较大、结构不完整,导致肿瘤血管通常包含有大量纳米尺度的小孔,使小分子和一些纳米颗粒能够透孔而出。目前已有很多研究利用肿瘤血管这种对小分子和纳米颗粒的高通透性来设计药物,通过控制药物颗粒合适的尺寸使其能够透过肿瘤血管进入瘤体,从而有效地提高抗肿瘤药物在肿瘤内的浓度。
王春儒团队研究发现,当纳米颗粒的尺度在合适的尺度下(例如50-200 nm),要经过几分钟甚至几十分钟才能通过肿瘤血管的间隙,在这一过程中纳米颗粒被肿瘤血管的内皮细胞所紧密包围,因此可以通过合适的设计而特异性地破坏肿瘤血管。首先,他们利用磁性金属富勒烯设计了尺度在150 nm左右的水溶性纳米颗粒,这种纳米颗粒的特性是能够通过吸收射频提高内能,在几分钟至几十分钟后由于内能升高发生相变,并伴随着体积剧烈膨胀50%左右。然后他们将金属富勒烯纳米颗粒静脉注入到小鼠体内,数分钟后这些纳米颗粒抵达肿瘤位置并长时间卡在血管壁上。这时他们再对小鼠施加射频“引爆”这些纳米颗粒。研究结果发现,这些镶嵌在肿瘤血管壁上的金属富勒烯纳米颗粒“爆炸”时有效地破坏了肿瘤血管,而后迅速阻断对于肿瘤的营养供应,几个小时内就可完全“饿死”肿瘤细胞。
因为几乎所有的肿瘤细胞都连接在肿瘤血管上,而正常细胞只连接在正常血管上,因此这种方法能够异常精准地杀灭肿瘤而对正常生物组织和器官无害,可称之为针对实体肿瘤的“分子手术刀”。实验发现,整个治疗过程快速、高效、低毒,而且对于肝癌、肺癌、乳腺癌等多种实体瘤均有显著疗效,是一种广谱的肿瘤治疗技术。目前该技术已经申请了国内和国际专利,正在进行临床前实验。相关研究成果最近在线发表在SCIENCE CHINA Materials(《中国科学:材料科学》上。
原文链接:
http://link.springer.com/article/10.1007/s40843-015-0089-3,
http://mater.scichina.com/EN/abstract/abstract509997.shtml)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












继续关注和学习
137
赞一个
152
太牛了
135
目前怎样
169
赞
158
会引起瘤体出血吗?
111
新技术
169