CDD:经门静脉自体骨髓输注有效逆转肝硬化,改善肝功能
2015-12-30 孙国根 医学论坛网
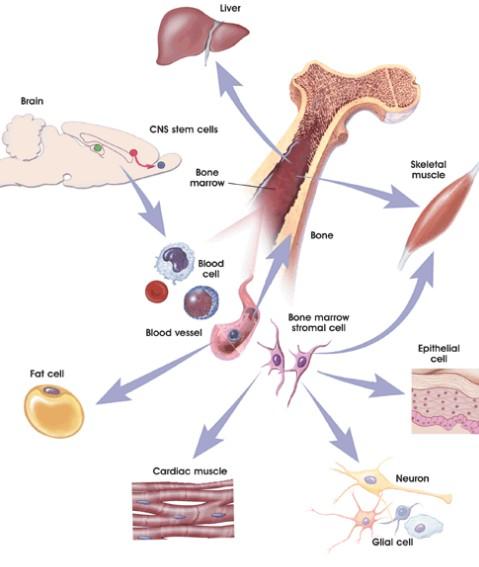
上海市公共卫生临床中心12月30日宣布, 经近5年努力,该中心普外一科主任刘保池教授率领的临床外科创新团队,应用肝硬化患者自体骨髓干细胞经门静脉回输的方法,使患者肝硬化得以逆转,腹水消失,黄疸消退,影像学检查发现原已缩至2分之一的肝脏体积增大,肝功能明显改善,并促进了患者的免疫重建。该成果已刊登在国际权威期刊《自然• 细胞死亡与疾病》(Cell Death & Disease)上。据了解,
上海市公共卫生临床中心12月30日宣布, 经近5年努力,该中心普外一科主任刘保池教授率领的临床外科创新团队,应用肝硬化患者自体骨髓干细胞经门静脉回输的方法,使患者肝硬化得以逆转,腹水消失,黄疸消退,影像学检查发现原已缩至2分之一的肝脏体积增大,肝功能明显改善,并促进了患者的免疫重建。该成果已刊登在国际权威期刊《自然• 细胞死亡与疾病》(Cell Death & Disease)上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#静脉#
69
不错,
159
不错,
160
感谢分享~~
151
感谢分享~~
135
好消息!
93
牛
146
专业
71
#肝功能#
65
#门静脉#
73