Clin Infect Dis: 婴儿期维生素D浓度和儿童期患结核病的风险
2022-06-27 xuyihan MedSci原创
小儿结核病指的是出生至16岁儿童所患结核病。小儿结核病的传染源主要是成人患者,尤其是家庭内传染极为重要,接触活动性肺结核患者的小儿的结核病感染率、发病率与患病率都较一般小儿显著为高。
每年有超过100万儿童患上结核病,发病率和死亡率都很高。儿童早期患结核病的风险最大,因此了解和确定哪些儿童处于高风险中对于针对有限的卫生资源并确定其优先级至关重要。在全球范围内,营养不良是导致结核病的主要原因,一些研究调查了微量营养素缺乏与结核病之间是否存在关联,结果不尽相同。在观察性研究中,在所有微量营养素缺乏症中,维生素D通常与结核病有关。结核病患者的维生素D浓度通常较低;然而,维生素D水平低是否能预测随后发生的结核感染或疾病尚不清楚。本项研究旨在探究婴儿期维生素 D 水平与整个儿童时期结核病随后发展之间的关系。

研究人员在南非儿童健康研究数据库中招募了处于妊娠20-28周的孕妇参加产前检查。然后在6-10周大的新生儿中测量血清 25(OH)D 浓度。使用每年的结核菌素皮肤试验、放射学检查和 GeneXpert 微生物诊断、培养和涂片检测对儿童的结核感染和疾病进行前瞻性跟踪。
本项研究结果显示儿童的结核病随访时间中位数为7.2年(IQR,6.2-7.9)。在744名儿童中(<1% 感染人类免疫缺陷病毒 (HIV),21% 接触过 HIV 未感染 HIV),婴儿早期维生素D缺乏的儿童患结核病的风险并未增加(HR,0.8;95%CI,0.4–1.6)。维生素D浓度最低三分位数的婴儿患结核病的风险与最高三分位数相似(HR,0.7;95%CI,0.4-1.4)。维生素D缺乏与≤2岁时的结核菌素阳性转化相关,截止值为<30nmol/L。
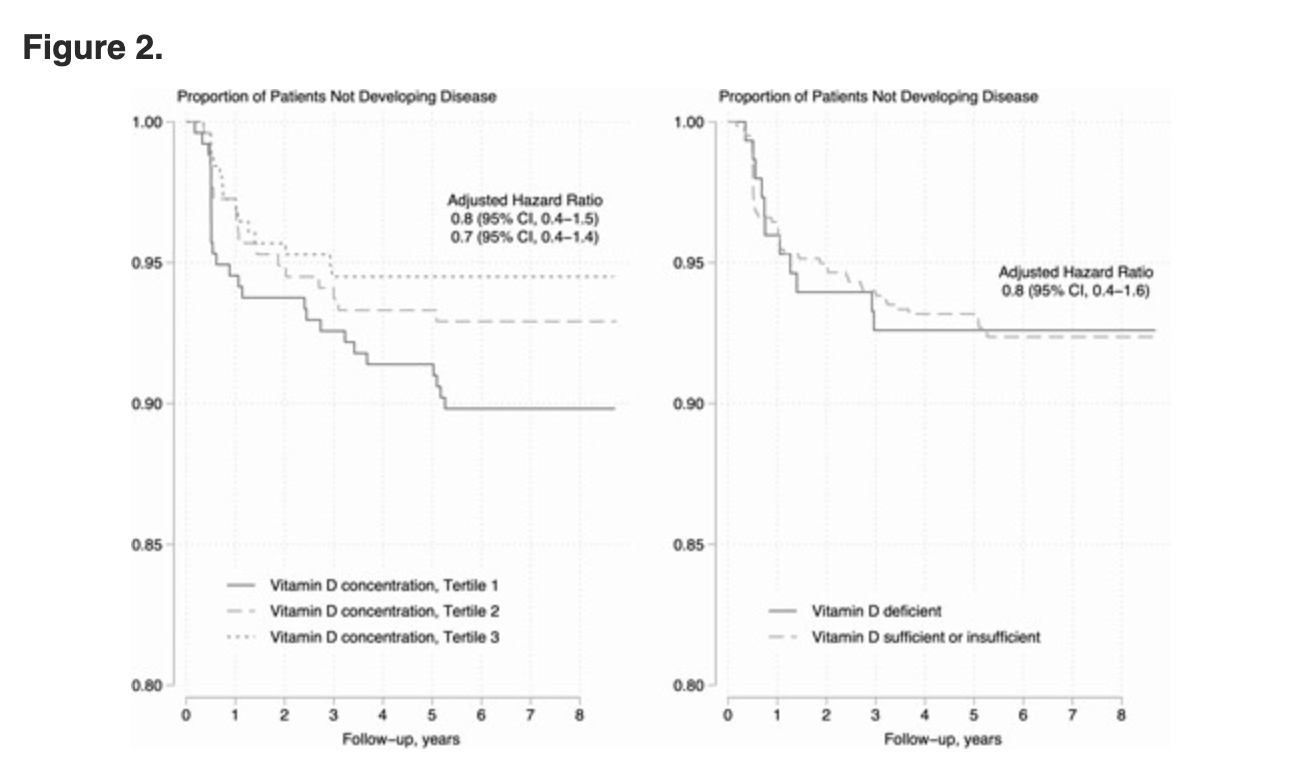
本项研究证实在结核病高流行的环境中,婴儿期的维生素D浓度并不能预测儿童期任何时候的结核病。然而,非常低的维生素 D 水平与幼儿的结核菌素转化有关。
原始出处:
Leonardo Martinez. Et al. Vitamin D Concentrations in Infancy and the Risk of Tuberculosis Disease in Childhood: A Prospective Birth Cohort in Cape Town, South Africa. Clinical Infectious Diseases.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Dis#
60
#结核#
91
#浓度#
75
#婴儿期#
68