J Hematol Oncol:「CAR-T疗效不佳」,可能是肿瘤微环境引发的T细胞衰老
2018-07-29 陈婉仪 医麦客
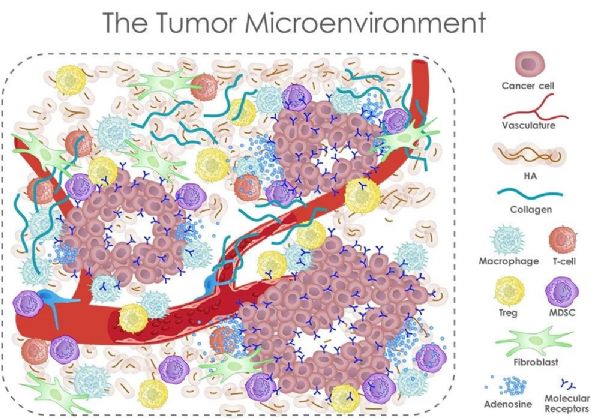
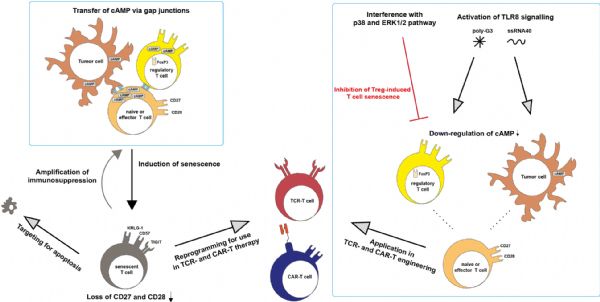
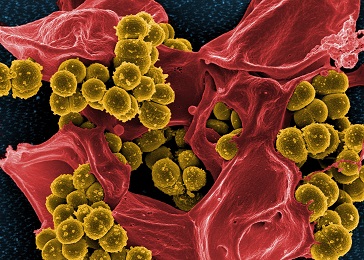
两款已经获批上市的CAR-T细胞疗法均需要从患者血液中提取T细胞,因此也称为自体CAR-T。目前,大多数癌症患者还没有从这些自体CAR-T疗法中获益,往往回收至体内的CAR-T细胞会出现肿瘤免疫逃逸现象,导致复发或治疗无效,因此也出现了与免疫检查点抑制剂(如PD-1/L1抗体)联合治疗等方案。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CAR-#
63
#Oncol#
77
a:¥CnTwb1llNAq¥
107
学习了
0
#EMA#
58
#细胞衰老#
71
学习了谢谢
115
谢谢梅斯提供这么好的信息,学到很多
82
理论研究越来越深入
108