氧化应激(OxS)和线粒体功能障碍被认为是衰老的原因。老年人(OA)的OxS升高、线粒体燃料氧化受损(MFO)、炎症升高、内皮功能障碍、胰岛素抵抗、认知功能下降、肌肉无力和骨质疏松症的发生率随着年龄的增长而增加,但其发生机制迄今尚不清楚,干预措施更是有限/缺乏。
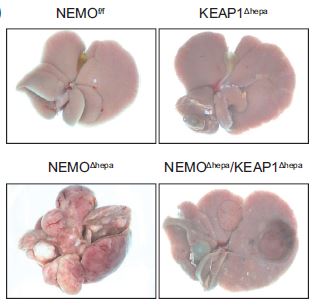
美国贝勒医学院Rajagopal V. Sekhar团队既往发现,在幼年小鼠中诱导抗氧化三肽谷胱甘肽(GSH)缺乏会导致线粒体功能障碍,而在老年小鼠中补充GlyNAC(甘氨酸和N-乙酰半胱氨酸[NAC]的组合物)可以改善自然发生的GSH缺乏、线粒体损伤、OxS和胰岛素抵抗。
近期,Rajagopal V. Sekhar团队的一项旨在测试补充和停用GlyNAC对细胞内GSH浓度、OxS、MFO、炎症、内皮功能、遗传毒性、肌肉和葡萄糖代谢、身体成分、力量和认知的影响的先导试验的研究论文发表在了“Clin Transl Med”上。
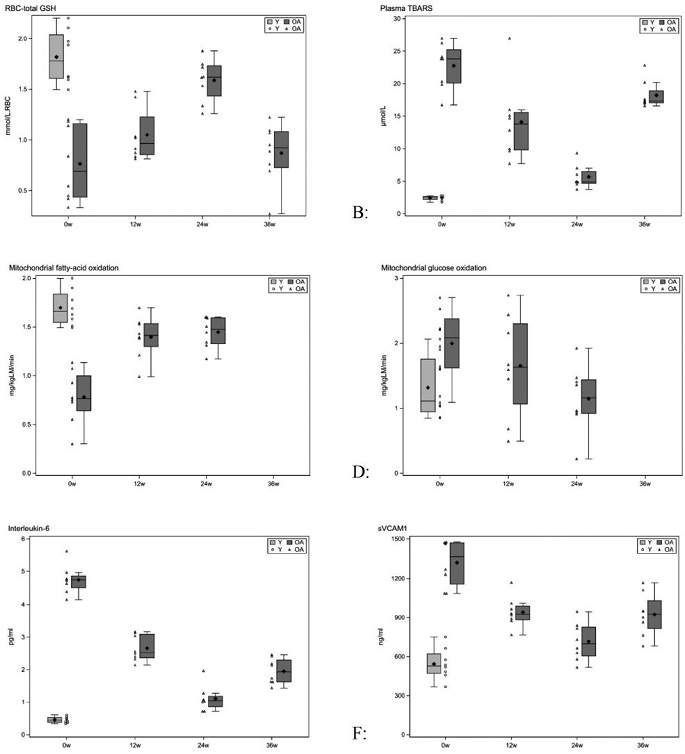
这是一项在8名老年人和8名青年人(YA)中进行了为期36周的开放标签的临床试验。在所有受试者都接受了初始(补充前)研究后,青年人终止了后续研究。在补充GlyNAC 24周和停用GlyNAC 12周后,再次对老年人进行评估。检测了红细胞(RBC)GSH、MFO与OxS、炎症、内皮功能、葡萄糖和胰岛素的生物标志物;还进行了步速、握力、6分钟步行试验,认知测试,基因组损伤,葡萄糖产生和肌肉蛋白质分解率以及身体成分分析。
补充GlyNAC和终止补充GlyNAC对各项指标的影响
补充GlyNAC 24周能够纠正老年人的RBC-GSH缺乏、OxS和线粒体功能障碍,改善炎症、内皮功能障碍、胰岛素抵抗、基因组损伤、认知、力量、步速和运动能力,降低体脂和腰围。然而,在停止补充GlyNAC12周后,上述获益消退。
综上,补充GlyNAC 24周对老年人的耐受性良好,降低了OxS,纠正了细胞内GSH缺乏和线粒体功能障碍,减轻了炎症、胰岛素抵抗和内皮功能障碍,减少了基因组损伤,改善了力量、步速、认知和身体成分。因此,予以老年人补充GlyNAC可能是一种简单可行的促进健康的方法,值得进一步研究。
原始出处:
Kumar Premranjan,Liu Chun,Hsu Jean W et al. Glycine and N-acetylcysteine (GlyNAC) supplementation in older adults improves glutathione deficiency, oxidative stress, mitochondrial dysfunction, inflammation, insulin resistance, endothelial dysfunction, genotoxicity, muscle strength, and cognition: Results of a pilot clinical trial. Clin Transl Med, 2021, 11: e372. https://doi.org/10.1002/ctm2.372
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Transl#
80
#TRA#
70
很好的研究
115
#Med#
82
谢谢
143
新突破,期待
120
氧化应激(OxS)和线粒体功能障碍被认为是衰老的原因。
114
棒棒哒
108