Neurology:未经证实的颈动脉血运重建获益患者斑块炎症与卒中复发的关联
2022-05-25 Naomi MedSci原创
近日,研究人员证实SCAIL 评分提高了在动脉内膜切除术试验中未获益的亚组中早期复发性卒中的识别。目前,还需要进行随机试验来测试联合狭窄-炎症策略是否会改善目前不确定益处的颈动脉血运重建的选择。
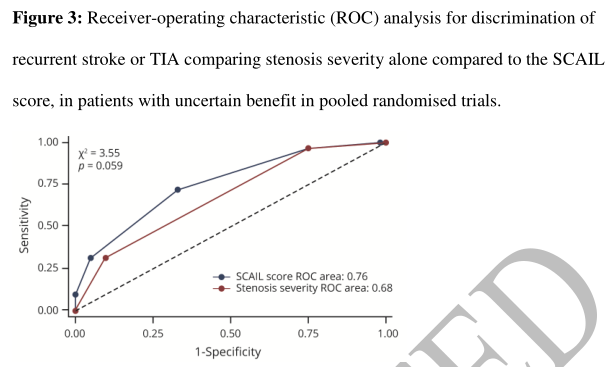
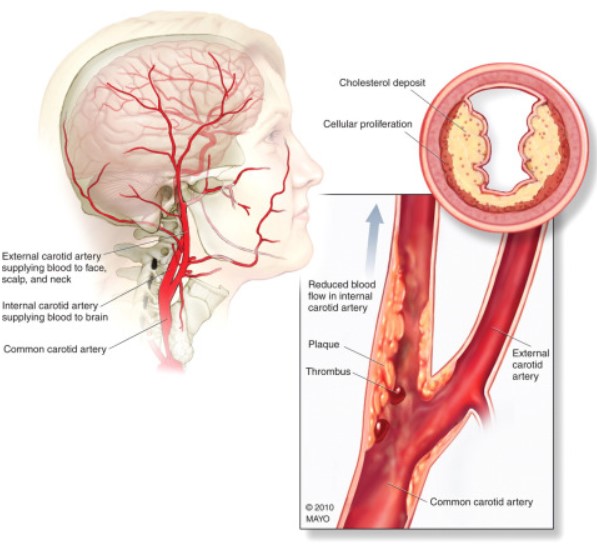
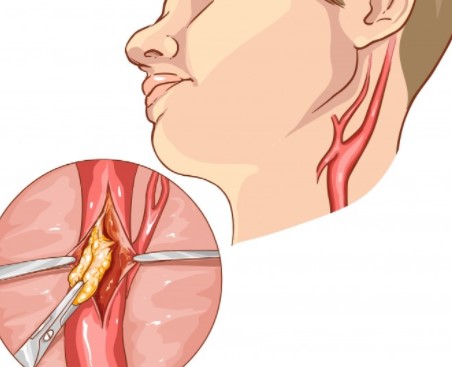
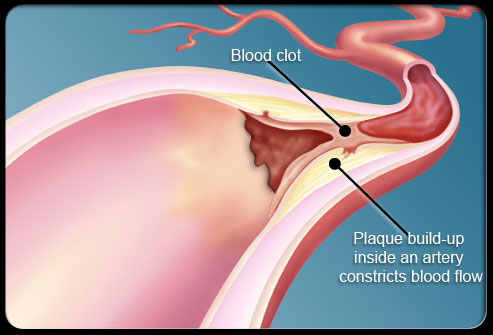
在对有症状颈动脉狭窄的动脉内膜切除试验的汇总分析中,几个亚组没有从血运重建中获得净获益。经验证的 SCAIL 评分包括通过正电子发射断层扫描 (PET) 测量的狭窄严重程度和炎症,与仅管腔狭窄相比,改善了对复发性卒中患者的识别。近日,研究人员调查了 SCAIL 评分是否提高了动脉内膜切除术试验中血运重建获益不确定的亚组中复发性卒中的识别。
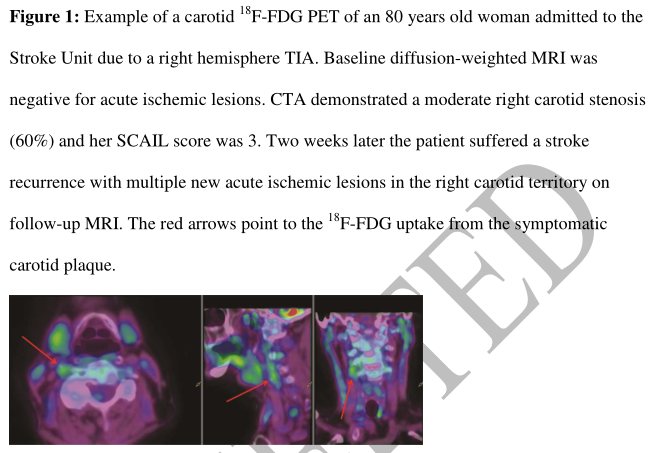
研究者对三项前瞻性队列研究(DUCASS,2008-2011;BIOVASC,2014-2018;巴塞罗那斑块研究,2015-2018)进行了个体参与者数据汇总分析。符合条件的患者近期发生过非严重(改良 Rankin 评分≤3)前循环缺血性卒中/TIA,并且:同侧轻度颈动脉狭窄(<50%);同侧颈动脉中度狭窄(50-69%)加上至少一种女性、年龄<65岁、糖尿病、TIA或血运重建延迟>14天;或单眼视力丧失。患者接受了联合登记的颈动脉18 F-FDG PET/CT 血管造影(纳入后≤7 天)。主要结局是90天同侧缺血性卒中。进行了多变量COX回归建模。
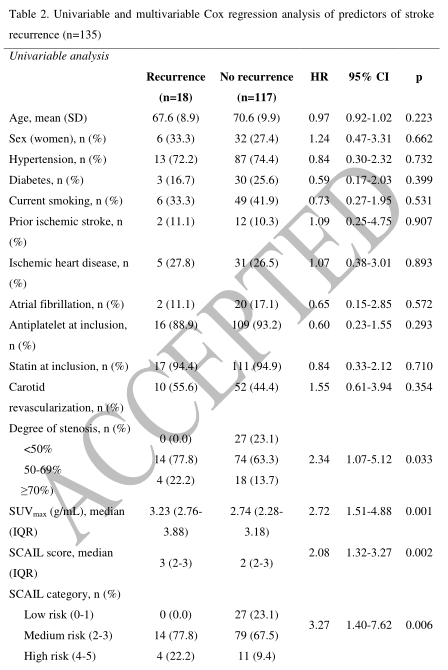
- 研究共纳入了 135 名患者。所有患者在入院时都开始了最佳的现代医学治疗,62 人(45.9%)接受了颈动脉血运重建(前 14 天内 36 人,之后 26 人)。
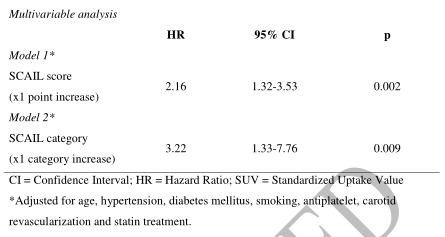
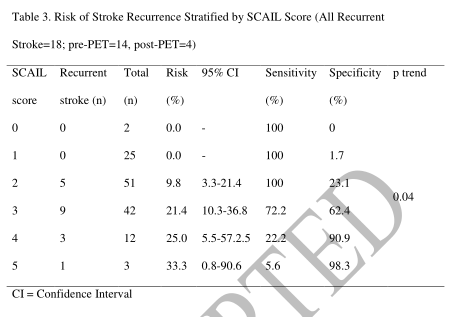
- 在 90 天时,18 名 (13.3%) 患者经历了至少一次卒中复发。根据 SCAIL 评分,复发风险逐渐增加(评分为 0-1 的患者为 0.0%,评分为 2-3 的患者为 15.1%,评分为 4-5 的患者为 26.7%;p=0.04)。
- 每增加 1 点 SCAIL 调整后(年龄、吸烟、高血压、糖尿病、颈动脉血运重建、抗血小板和他汀类药物)同侧复发性卒中的风险比为 2.16(95% CI 1.32-3.53;p=0.002)。
- 评分≥2 对复发的敏感性为 100%。
SCAIL 评分提高了在动脉内膜切除术试验中未获益的亚组中早期复发性卒中的识别。需要进行随机试验来测试联合狭窄-炎症策略是否会改善目前不确定益处的颈动脉血运重建的选择。
证据分类: 本研究提供的 II 类证据表明,在近期患有前循环缺血性卒中且未从颈动脉血运重建中受益的患者中,SCAIL 评分可准确区分有复发性同侧缺血性卒卒中险的患者。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#颈动脉#
73
#动脉血#
60
#血运重建#
117
#Neurol#
89
#斑块#
65
#卒中复发#
0