JAHA:经胸超声心动图诊断肺动脉高压近一半可能存在漏诊
2018-07-02 MedSci MedSci原创
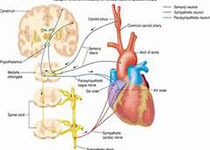
经胸超声心动图(TTE)可以用来测量肺动脉收缩压,但需要用来计算肺动脉收缩压的三尖瓣反流速度(TRV)常常不能被测量。目前TRV不能被测量是否意味着肺动脉收缩压正常尚属未知。本研究纳入了1998年至2014年行右心导管术的患者,分析了其血液动力学、TTE和临床资料,肺动脉高压(PH)定义为肺动脉压力≥25mmHg。最终共纳入分析了1262名行右心导管术后2天内接受了TTE检查的患者,有803名(6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#心动图#
66
#经胸超声心动图#
106
#动脉高压#
70
#AHA#
65
#漏诊#
65
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
73
学习了.好文章.
83
尴尬
94
学习了.长知识
84