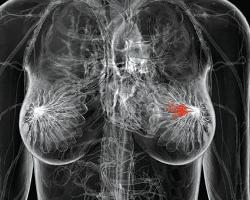
JNCI:预测乳腺癌患者的预后的新方法
2015-07-27 徐媛媛译 MedSci原创
背景:以往研究表明,对HER2的胞内结构域(ICD)和胞外结构域(ECD)使用传统治疗方法的抗体疗效是一样的。本研究采取了一个新的方法来分别定量ICD和ECD的表达,以评估接受曲妥珠单抗辅助治疗的患者的HER2特定结构域的预测价值。 方法:研究人员通过在组织芯片上使用两种抗体--抗ICD抗体(CB11 和A0485)和抗ECD抗体(SP3和D8F12),再通过定量免疫荧光技术(QIF)来检测HE
背景:以往研究表明,对HER2的胞内结构域(ICD)和胞外结构域(ECD)使用传统治疗方法的抗体疗效是一样的。本研究采取了一个新的方法来分别定量ICD和ECD的表达,以评估接受曲妥珠单抗辅助治疗的患者的HER2特定结构域的预测价值。
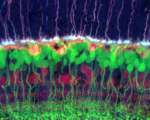
方法:研究人员通过在组织芯片上使用两种抗体--抗ICD抗体(CB11 和A0485)和抗ECD抗体(SP3和D8F12),再通过定量免疫荧光技术(QIF)来检测HER2的表达。研究人员检测了来自于辅助化疗加曲妥珠单抗的临床试验的180名患者的ICD和ECD的表达,并对预测值进行了评估(HeCOG 10/05)。研究人员使用Kaplan-Meier评估功能对无病生存期(DFS)进行分析。统计测试都是双面的。
结果:通过QIF检测HER2的ICD表达比ECD表达的敏感性较高,而且更具体,有较高的阳性预测值。在HeCOG 10/05试验的样本中,有15%表现出ICD与ECD表达的差异。ECD高表达显示出更久的DFS(log-rank P=0.049,HR=0.31,95%CI=0.144-0.991),ICD表达则没有预测效果。在ECD低表达的患者中,ICD的高低对DFS无影响。而当ICD高表达时,ECD高表达患者与低表达患者的DFS则有显著性差异,ECD高表达患者有更久的DFS(log-rank P=0.027,HR=0.23,95%CI=0.037-0.82)。
结论:对乳腺癌患者HER2的ICD和ECD进行定量检测显示HER2阳性乳腺癌患者中存在亚型。接受曲妥珠单抗治疗的患者中,ECD高表达的患者显示出了更好的DFS。这表明ECD表达量不同,应用曲妥珠单抗治疗的获益也存在差异。对ECD表达量的检测能更好的预测曲妥珠单抗的治疗效果。
原始出处
Carvajal-Hausdorf DE1, Schalper KA1, Pusztai L1, Psyrri A1, Kalogeras KT1, Kotoula V1, Fountzilas G1, Rimm DL2.Measurement of Domain-Specific HER2 (ERBB2) Expression May Classify Benefit From Trastuzumab in Breast Cancer.J Natl Cancer Inst. 2015 May 19
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#新方法#
64
#NCI#
59
#乳腺癌患者#
57
挺新颖
159