Eur Radiol:看一看乳腺癌患者哨卫淋巴结有没有转移?
2017-12-23 shaosai MedSci原创
本研究旨在验证增强超声(CEUS)在乳腺癌术前识别哨卫淋巴结(SLN)的可行性及增强模式在诊断淋巴结转移和腋窝淋巴结负荷的特点,并将结果发表在Eur Radiol上。
本研究旨在验证增强超声(CEUS)在乳腺癌术前识别哨卫淋巴结(SLN)的可行性及增强模式在诊断淋巴结转移和腋窝淋巴结负荷的特点,并将结果发表在Eur Radiol上。
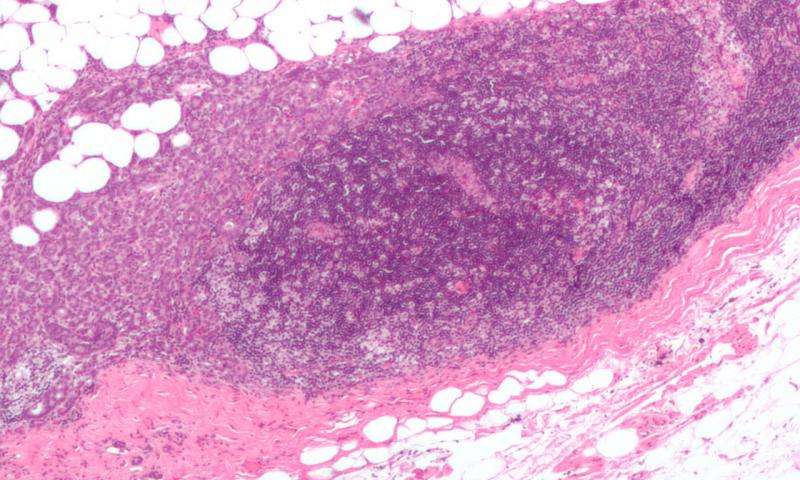
本研究共纳入了110例乳腺癌患者。在术前,对患者进行皮下注射微泡造影剂。检查淋巴引流路径来识别SLNs。利用蓝染法和吲哚菁绿在术中追踪SLNs。记录SLN的强化模式并与最终病理结果相比较。
结果为,110例患者中SLN的检出率为96.4%,共检出134个SLN。通过CEUS增强模式预测SLN转移的敏感性、特异性、阳性预测值、阴性预测值和准确率分别为100 %、52.0 %、43.4 %、100 % 、64.9 %。非转移性SLN表现为均一强化。有0-2SLN转移的低结节负荷在92.5%的结节中表现为不均质强化。在100%的无强化模式的病人中均被证实有SLN转移。
本研究表明,CEUS是一种识别SLN可行的方法。CEUS增强模式有助于识别转移性SLN及结节负荷。
原始出处:
Zhao J, Zhang J, Zhu QL. et al.The value of contrast-enhanced ultrasound for sentinel lymph node identification and characterisation in pre-operative breast cancer patients: A prospective study.Eur Raidol.DOI: 10.1007/s00330-017-5089-0
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#哨卫淋巴结#
83
一起学习学习
90
#淋巴结#
78
#乳腺癌患者#
66
学习
106
学习
77
阅
107