CHEST:超声检查或可减少肺栓塞诊断时的CTPA滥用
2013-12-24 佚名 丁香园
CT肺血管造影(CTPA)一直被看作是诊断肺栓塞(PE)的金标准,并经常被用于一些以心、肺症状为主诉的患者。然而,不加选择地滥用CTPA会显著增加患者对电离辐射和造影剂的暴露。为了评估利用床边超声检查来预测CTPA必要性的方案是否可靠,来自美国霍夫斯特拉北岸长岛犹太医疗中心的Seth Koenig等人进行了一项研究,研究结果在线发表于2013年10月31日的CHEST杂志上
CT肺血管造影(CTPA)一直被看作是诊断肺栓塞(PE)的金标准,并经常被用于一些以心、肺症状为主诉的患者。然而,不加选择地滥用CTPA会显著增加患者对电离辐射和造影剂的暴露。为了评估利用床边超声检查来预测CTPA必要性的方案是否可靠,来自美国霍夫斯特拉北岸长岛犹太医疗中心的Seth Koenig等人进行了一项研究,研究结果在线发表于2013年10月31日的CHEST杂志上。结果显示:超声检查或可减少肺栓塞诊断时CT肺血管造影的滥用。
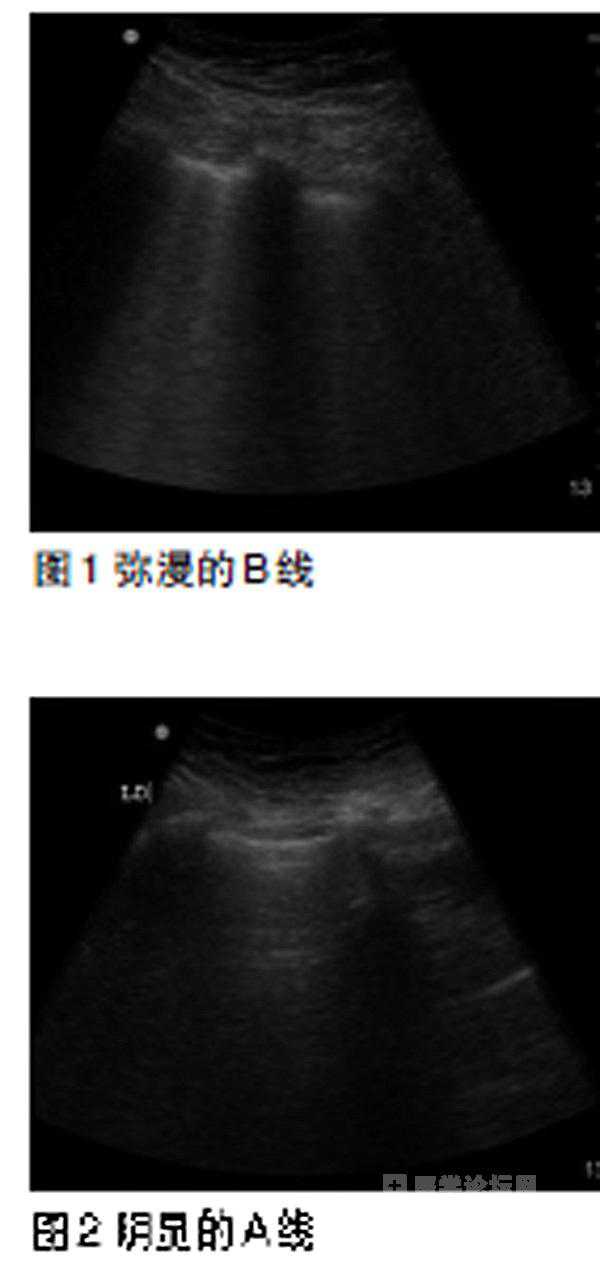
该项观察性研究主要由受过危重症救护超声检查训练的呼吸和危重症医学科医生实施。研究者对那些申请以CTPA来除外PE诊断的患者先进行了超声筛查。超声检查的项目包括适度的心脏超声检查、胸部超声检查、和下肢深静脉的加压超声检查等。如果超声发现患者有深静脉血栓形成;或发现患者为其它疾病有明确证据,研究者即预计该患者的CTPA没有必要进行。研究者将超声筛查结果,与受试者肺实质和胸膜的CTPA结果、及其可用的、正式深静脉血栓和心脏超声检查结果等进行了对比研究。
该研究的主要结果为:在96例接受了CTPA检查的受试者中,有12人(12.5%)被证实为PE.这96例受试者均接受了超声筛查,其中2人(2.1%)超声检查发现了下肢深静脉血栓,54人(56.2%)超声检查提示其为其它疾病,例如,发现了符合肺炎或肺水肿的肺泡实变超声表现等。上述54例受试者的肺部超声检查结果与其CTPA检查结果基本一致,CTPA检查没能在超声筛查的基础上再发现任何新的诊断。
该研究显示:①根据超声检查结果,上述96例受试者中的56例(58.3%)并无行CTPA检查的必要。②一个关注检查部位的超声筛查方案或能预测出哪些患者需行CTPA检查。③超声检查可以明确患者可能的其它诊断,而且其在这方面的诊断效果与CTPA基本一致。研究者认为,尽管上述研究还需进一步验证,但其为人们提供了一种减少CTPA使用、和电离辐射暴露的可能方法。
原文出处:
Seth Koenig, MD, FCCP; Subani Chandra, MD; Artur Alaverdian, MD; Christopher Dibello, MD; Paul H. Mayo, MD, FCCP; Mangala Narasimhan, DO, FCCP.Ultrasound Assessment of Pulmonary Embolism in Patients Receiving Computerized Tomography Pulmonary Angiography.Chest. 2013. doi:10.1378/chest.13-0797
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#tPA#
78
#CTP#
77
#EST#
70
疑诊PE,先做超声检查
138
#Chest#
61
#滥用#
80
#超声检查#
64
#CTPA#
76