Ann Intern Med:切除甲状旁腺对轻度甲状旁腺功能亢进患者发病率和死亡率的影响
2022-04-20 Nebula MedSci原创
切除甲状旁腺对轻度甲状旁腺功能亢进患者无明显效益。
原发性甲状旁腺功能亢进 (PHPT) 是一种常见的内分泌疾病,与骨折、心血管疾病、肾脏疾病和癌症的风险增加和死亡率增加有关。PHPT还是非住院患者高钙血症最常见的原因。几十年来,无症状、轻微的PHPT是否会增加总体死亡率和心血管疾病 (CVD) 风险一直存在争议。
因缺乏长期随机试验数据,伴轻度高钙血症且无已知疾病的轻度PHPT患者是否需要进行甲状旁腺切除术(PTX)仍存在争议。
本研究是一项前瞻性随机对照试验,旨在评估甲状旁腺切除术对轻度PHPT患者死亡率(主要终点)和重要疾病发病率(次要终点)的影响。
纳入了1998年-2005年期间就诊的191位轻度PHPT患者,随机分至两组:PTX组 95位,观察组(OBS)96位。随机分组10年后从瑞典和挪威死亡原因登记处采集死亡日期及原因,并延长观察至2018年。
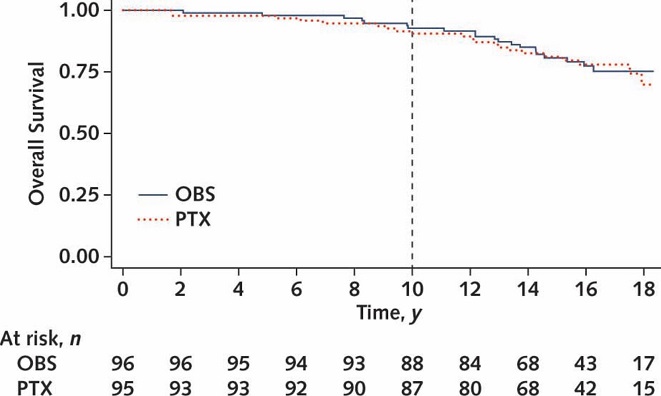
两组的总生存率
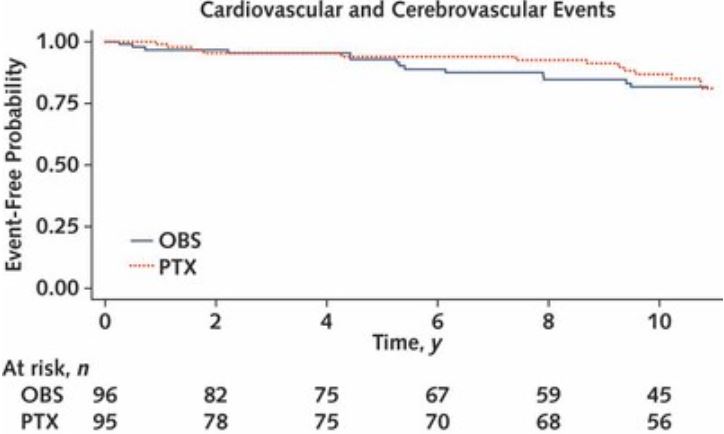
随机分组10年内,有15位患者死亡(PTX组 8位,观察组 7位)。在延长观察期间,共发生了44例死亡(PTX组 24例,观察组 20例)。共有101例发病事件(包括心血管事件、脑血管事件、癌症、四肢骨折和肾结石),在两组间的发生率相近(PTX组 52例,观察组 49例)。在研究期间,有14位患者共发生了16例椎体骨折(每组各7位)。
两组无心血管和脑血管事件生存率
综上,甲状旁腺切除术似乎不能降低轻度PHPT的发病率或死亡率。至少在10年时间里,没有观察到与死亡、骨折、癌症、心脑血管事件或肾脏相关疾病发生率相关不良影响的证据。
原始出处:
Pretorius Mikkel,Lundstam Karolina,Heck Ansgar et al. Mortality and Morbidity in Mild Primary Hyperparathyroidism: Results From a 10-Year Prospective Randomized Controlled Trial of Parathyroidectomy Versus Observation.[J] .Ann Intern Med, 2022, https://doi.org/10.7326/M21-4416.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#发病率#
53
#甲状旁腺功能亢进#
66
#甲状旁腺#
53
#Med#
48