Nat Med:癌症患者白细胞抗原种类越多免疫疗效越好
2019-11-12 不详 新华网
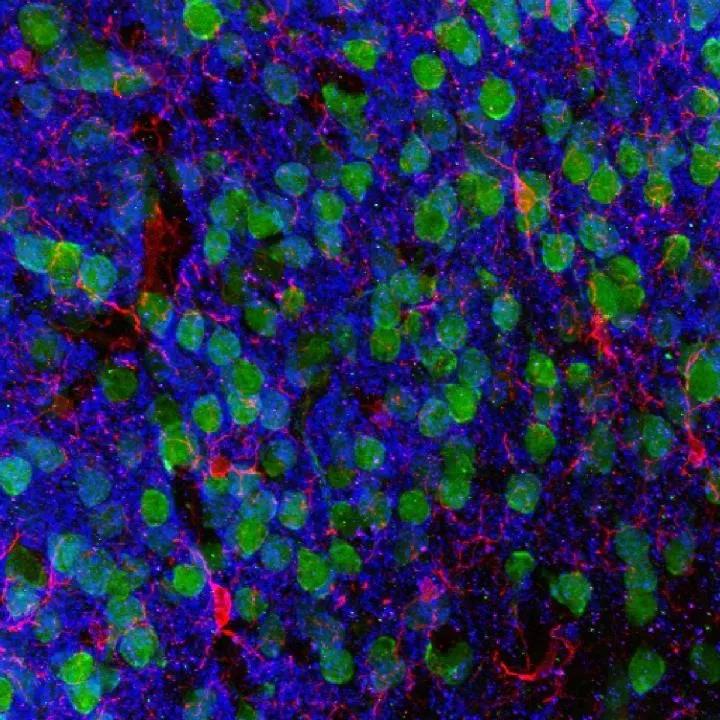
新一期英国《自然·医学》日前刊载的一项研究发现,癌症患者体内白细胞抗原种类越多,其接受免疫治疗的效果越好。未来医生有望根据癌症患者的人类白细胞抗原基因图谱,提供更好的个体化治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
80
#癌症患者#
0
#Med#
69
#抗原#
90
谢谢梅斯提供这么好的信息,学到很多
0