Crit Care:血小板与淋巴细胞比值对急性肾损伤患者预后的预测价值如何?
2017-10-21 xing.T MedSci原创
在AKI患者中,术前PLR与生存率之间存在U形相关。PLR似乎是患有AKI危重病患者一个新的独立预后指标。
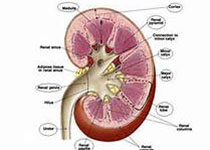
炎症在急性肾损伤(AKI)的发生和发展中起着重要的作用。然而,关于血小板与淋巴细胞比率(PLR),一种全身性炎症标志物,在AKI患者中预后效应的证据较少。近日,危重病医学领域权威杂志Critical Care上发表了一篇研究文章,在这项研究中,研究人员调查了PLR在患有AKI的危重患者预后预测中的价值。
研究人员从重症监护病房数据库中提取病人数据,采用光滑曲线拟合来测定PLR的临界值,并对这些患者进行分组。其临床结果为ICU内30天和90天的死亡率。研究人员使用Cox比例风险模型来评估PLR和患者生存之间的相关性。
该研究共纳入10859例发AKI的ICU患者。在30天和90天共有2277例和3112例患者死亡。PLR和90天和30天死亡率之间均呈U型关系,最低的风险值变化范围从90到311。考虑到风险值 < 90和 > 311,90天死亡率调整后的风险比(95%可信区间)分别为1.25(1.12-1.39)和1.19(1.08-1.31)。30天死亡率也可以观察到类似的趋势。PLR和年龄以及心率之间的相互作用也发现具有统计学意义。只有当PLR<90时,年轻(年龄<65岁)和心率较快(≥89.4次/分)的患者往往有较差的预后,而只有当PLR>311时,老年(年龄≥65岁)与心率较慢(<89.4次/分)具有较高的风险(对于年龄P<0.001;对于心率P<0.001)。
由此可见,在AKI患者中,术前PLR与生存率之间存在U形相关。PLR似乎是患有AKI危重病患者一个新的独立预后指标。
原始出处:
Chen-Fei Zheng,,et al. Prognostic value of platelet-to-lymphocyte ratios among critically ill patients with acute kidney injury.Critical Care.2017. https://doi.org/10.1186/s13054-017-1821-z
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#患者预后#
39
#淋巴细胞#
36
#损伤#
36
#预测价值#
41
学习了.谢谢分享.
59