J Periodontol:甲硝唑联合阿莫西林治疗伴2型糖尿病的牙周炎患者:一项随机对照试验随访 5 年的二次分析结果
2021-08-13 MedSci原创 MedSci原创
已知糖尿病(DM)是牙周炎的危险因素,最近的系统回顾显示,在治疗牙周炎和2型糖尿病患者时,使用全身性抗生素作为洁治和根面平整术(SRP)的辅助治疗,比仅使用SRP的临床效益更佳。
已知糖尿病(DM)是牙周炎的危险因素,最近的系统回顾显示,在治疗牙周炎和2型糖尿病患者时,使用全身性抗生素作为洁治和根面平整术(SRP)的辅助治疗,比仅使用SRP的临床效益更佳。
近日,发表于J Periodontol的一项新的研究报道了既往发表的一项随机试验(RCT)5年随访分析结果,表明甲硝唑(MTZ)加阿莫西林(AMX)作为洁治和根管治疗(SRP)的辅助疗法可有效治疗2型糖尿病患者的牙周炎。
研究选择在上述RCT中接受牙周治疗的志愿者进行临床和微生物学评估。患者在治疗后2至5年内没有接受定期的支持性牙周治疗(SPT)。
在参加RCT的患者中,43%进入本研究分析(n = 10/对照组和15/测试组)。与抗生素治疗组的基线相比,大多数临床参数值,包括探诊深度≥5mm的部位数量(主要结果变量),在治疗后5年都有所下降(P < 0.05),但呈现出比2年时更高的数值(P < 0.05)。治疗后5年,MTZ+AMX+SRP组和仅SRP组的微生物复合体的平均比例没有差异(P>0.05)。
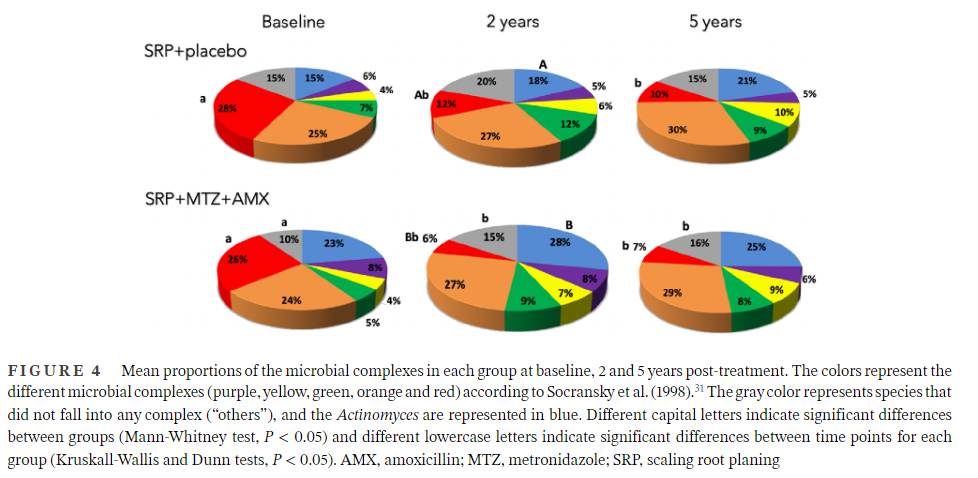
综上所述,该研究结果表明,MTZ+AMX辅助治疗比仅SRP治疗伴牙周炎的糖尿病患者在5年内的维持治疗效果更好。然而,在治疗后 2 - 5 年间未接受 SPT 的这些患者中,治疗后获得的长达 2 年的临床和微生物学益处并未完全持续。
原始出处:
Daniele Ferreira da Cruz, et al., Metronidazole and amoxicillin for patients with periodontitis and diabetes mellitus: 5-year secondary analysis of a randomized controlled trial. J Periodontol. 2021 Apr;92(4):479-487. doi: 10.1002/JPER.20-0196.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#对照#
94
#PE#
89
#对照试验#
79
#随机对照试验#
76
#甲硝唑#
87
#牙周#
97
学习了
150
高质量研究,读起来真爽,谢谢梅斯
133
谢谢MedSci提供最新的资讯
129