Diabetologia:超声心动图提高了对1型糖尿病和无已知心脏病人群主要不良心血管事件的预测?
2019-12-28 MedSci MedSci原创
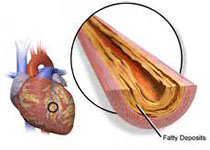
心血管疾病是1型糖尿病最常见的共患病。然而,目前的指南不包括心肌功能的常规评估。在此,我们研究了超声心动图是否为没有已知心脏病的1型糖尿病患者提供增量预后信息。
心血管疾病是1型糖尿病最常见的共患病。然而,目前的指南不包括心肌功能的常规评估。在此,我们研究了超声心动图是否为没有已知心脏病的1型糖尿病患者提供增量预后信息。
我们从门诊招募了一组没有已知的心脏病1型糖尿病患者。通过丹麦国家登记册进行随访。 观察超声心动图与主要心血管不良事件(MACE)的关系以及在临床StenoT1D危险中增加预后的价值。
本研究共纳入1093人:中位(四分位范围)年龄为50.2(39.2-60.3)岁,糖化血红蛋白65
(56-74)mmol/mol;男性53%;平均BMI (SD)为25.5
(3.9)kg/m2,平均糖尿病病程为25.8(14.6)年。在7.5年的随访中,145人(13.3%)出现了MACE。超声心动图显著独立预测心肌梗死:左室射血分数(LVEF)
<45% (n = 18) vs≥45% (n = 1075), HR (95% CI)
3.93 (1.91, 8.08), p <
0.001;整体纵向应变受损(GLS), 1.65 (1.17,
2.34) (n = 263), p = 0.005;舒张期二尖瓣早期速度(E)/舒张期早期组织多普勒速度(E’)<8 (n
= 723) vs E/ E’8 - 12 (n = 285), 1.59 (1.04,
2.42), p = 0.031;和E / E′< 8
vs E / E′≥12 (n = 85), 2.30 (1.33, 3.97), p = 0.003。在LVEF保留的个体中(n = 1075),GLS受损的估计值为1.49(1.04,2.15),p = 0.032; E / e'<8
vs E / e'8-12,1.61(1.04,2.49),p = 0.033; 和E / e'<8
vs E / e'≥12,2.49(1.41,4.37),p = 0.001。 在Steno T1D风险引擎中添加超声心动图变量可以显着改善风险预测:Harrell的C统计量为0.791(0.757,0.824)对0.780(0.746,0.815),p = 0.027; 净重分类指数为52%,p <0.001。
研究结果表明,在没有已知心脏病的1型糖尿病患者中,超声心动图可显著提高风险预测,而不仅仅是指南推荐的临床风险因素,并可在临床护理中发挥作用。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#心动图#
51
#BET#
56
#DIA#
65
#血管事件#
70
#主要不良心血管事件#
144
谢谢MedSci提供最新的资讯
67