这种病不常见 极易误诊为特发性肺动脉高压
2018-03-29 熊长明 肺血管病
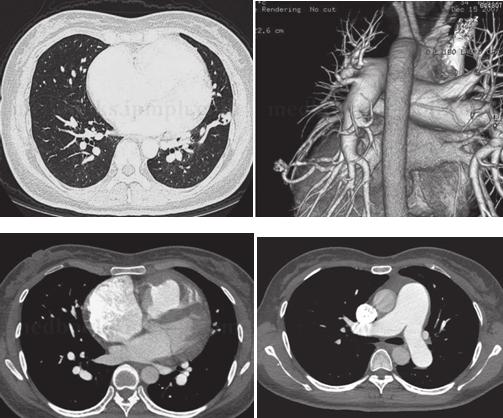
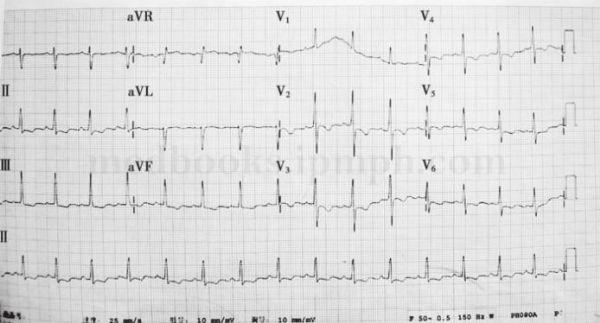
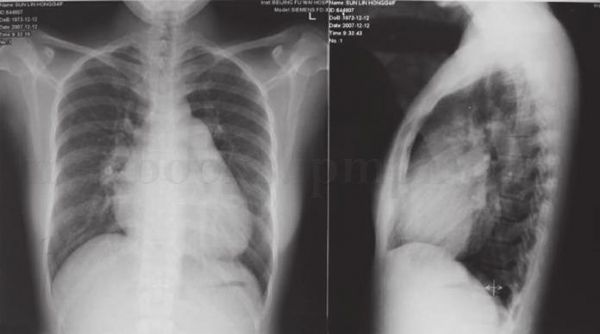
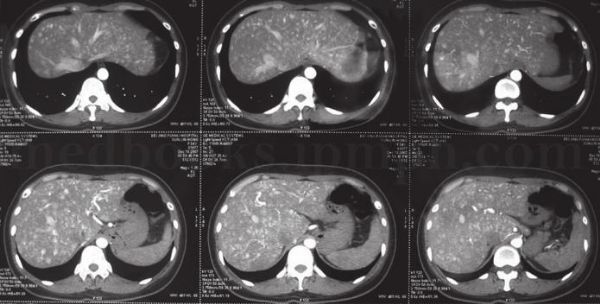
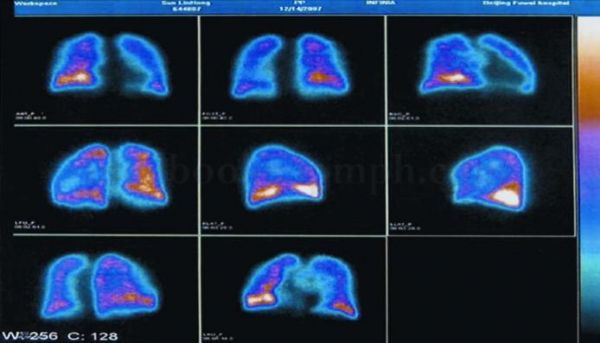
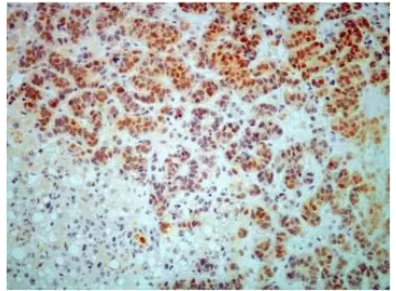
患者,女,34岁。既往有较大活动后气短、胸闷史,未予以重视。6个月前出现间断咯血,无发热,被当地医院诊断为肺动脉高压。患者既往有反复鼻出血史;反复黑便,贫血。其父亲及一姐均有反复鼻出血史。患者肺动脉高压到底是何种疾病引起?是特发性肺动脉高压吗?详见以下病例。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#动脉高压#
125
#特发性肺动脉高压#
130
#特发性#
160
学习了谢谢分享!!
158
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
175
谢谢分享学习一下
153