EHRA 2021|LBCTs 先睹为快!RACE 3:持续性心房颤动和轻中度稳定型心力衰竭患者潜在疾病的靶向治疗的长期结果
2021-04-19 “心关注”公众号 “心关注”公众号
RACE 3研究的目的是探讨早期持续性心房颤动和轻中度早期心力衰竭患者是否采用积极的上游心律控制方法,包括醛固酮受体拮抗剂和他汀类药物、饮食限制、咨询和心脏康复计划,与常规心律控制相比,随访一年后窦性
RACE 3研究的目的是探讨早期持续性心房颤动和轻中度早期心力衰竭患者是否采用积极的上游心律控制方法,包括醛固酮受体拮抗剂和他汀类药物、饮食限制、咨询和心脏康复计划,与常规心律控制相比,随访一年后窦性心律的持续性增加。
将对RACE研究进行5年的总随访,以研究两种治疗策略对窦性心律持续性和心血管发病率及死亡率的长期影响。
DESIGN
EHRA 2021 · RACE 3
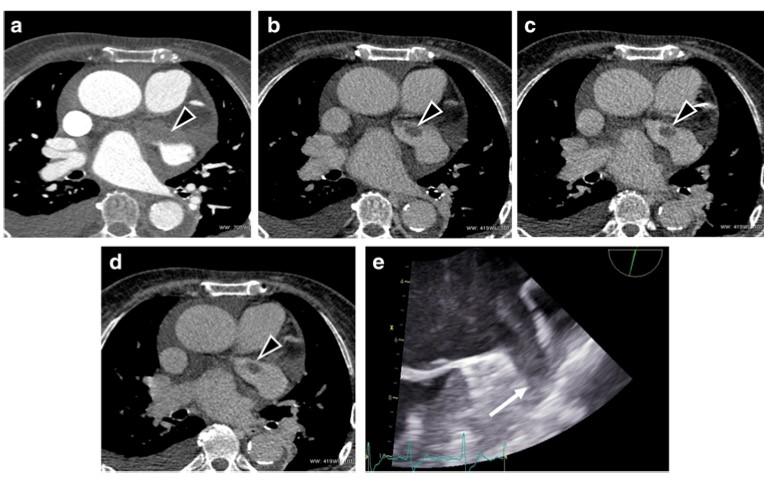
图片研究设计于2013年发表于Neth Heart J。
Background
心房颤动(AF)的心律控制是很复杂的,因为它是由结构重建引起的进行性的。上游治疗是指旨在改变心房基底的治疗性干预,从而预防房颤。
Objective
预防心力衰竭早期房颤的常规与强化上游心律控制(RACE 3)的研究假设,在接受电复律的早期房颤和轻度至中度早期收缩或舒张性心力衰竭患者中,强化上游心律控制较传统心律控制增加窦性心律的持续性。
Design
RACE 3为前瞻性、随机、开放、多国、多中心试验。上游节律控制包括血管紧张素转换酶抑制剂和/或血管紧张素受体阻滞剂、盐皮质激素受体拮抗剂、他汀类药物、心脏康复治疗以及关于饮食限制、运动维持和药物依从性的强化咨询。常规心律控制包括常规心律控制治疗,无需心脏康复治疗和强化咨询。在两臂中,尽一切努力保持患者的心律控制策略,如果房颤复发,可以使用离子通道抗心律失常药物或肺静脉消融。总共包括250名患者。如果上游治疗能有效改善窦性心律的维持,它将成为一种新的心律控制方法,支持传统的药物和非药物心律控制。
今年EHRA 2021上将公布一研究的长期随访结果。北京时间:04月23日23:55。
Eur Heart J
RACE 3 · 2018
图片2018年在European Heart Journal上刊登的结果显示:研究证实了潜在疾病的靶向治疗可以改善患者的窦性心律维持持续性房颤。研究发现在短时间房颤和心衰的患者中,针对基础疾病的靶向治疗对降低血压和血脂水平以及改善心衰有价值。
Methods and results
我们将早期持续性房颤和轻中度心力衰竭(HF)患者随机分为基础疾病靶向治疗组和常规治疗组。两组均接受房颤和心衰的因果治疗和心律控制治疗。在干预组中,除此之外,开始了四种疗法:(i)盐皮质激素受体拮抗剂(MRA),(ii)他汀类药物,(iii)血管紧张素转换酶抑制剂和/或受体阻滞剂,以及(iv)心脏康复,包括体力活动、饮食限制和咨询。主要终点是动态心电图监测7天时1年的窦性心律。245例患者中,119例随机分为靶向治疗组和126例常规治疗组。干预导致MRA(101[85%]对5[4%]患者,P?<?0.001)和他汀类药物使用(111[93%]对61[48%],P?<?0.001)的对比。血管紧张素转换酶抑制剂/血管紧张素受体阻滞剂无差异。109例(92%)患者完成了心脏康复。干预组的基础疾病得到了更成功的治疗。1年时,干预组有89例(75%)患者出现窦性心律,而常规组有79例(63%)(比值比1.765,95%可信区间下限1.021,P?=?0.042)。

Europace
RACE 3 · 2019
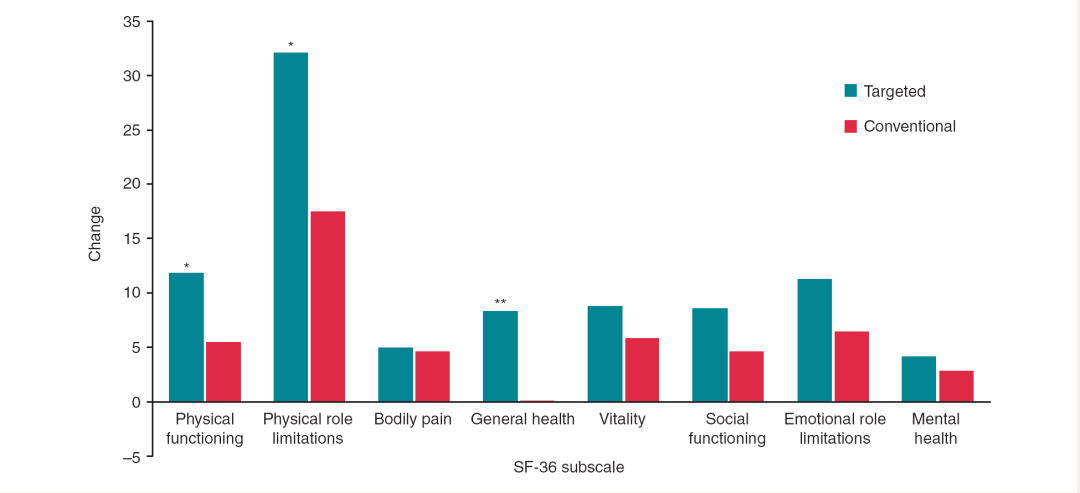
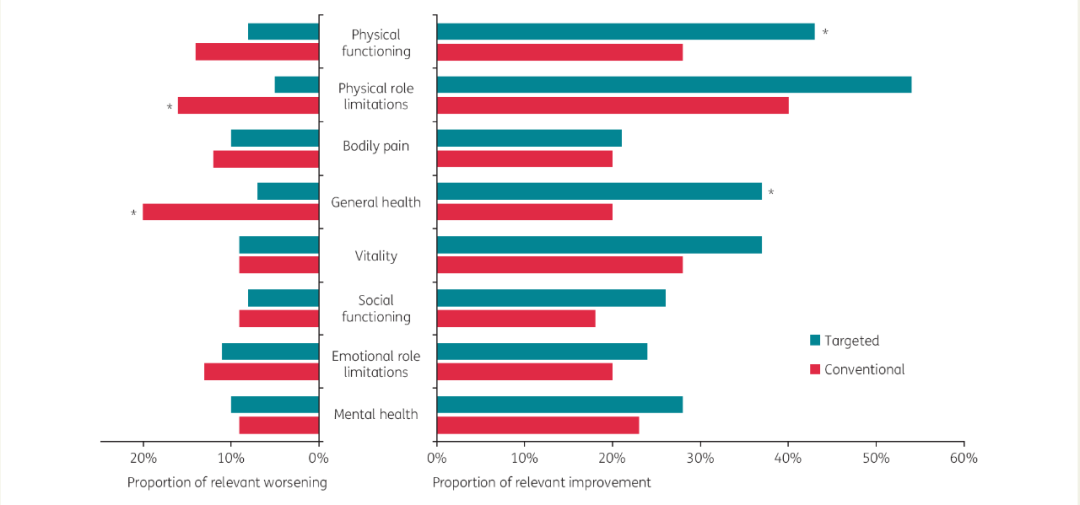
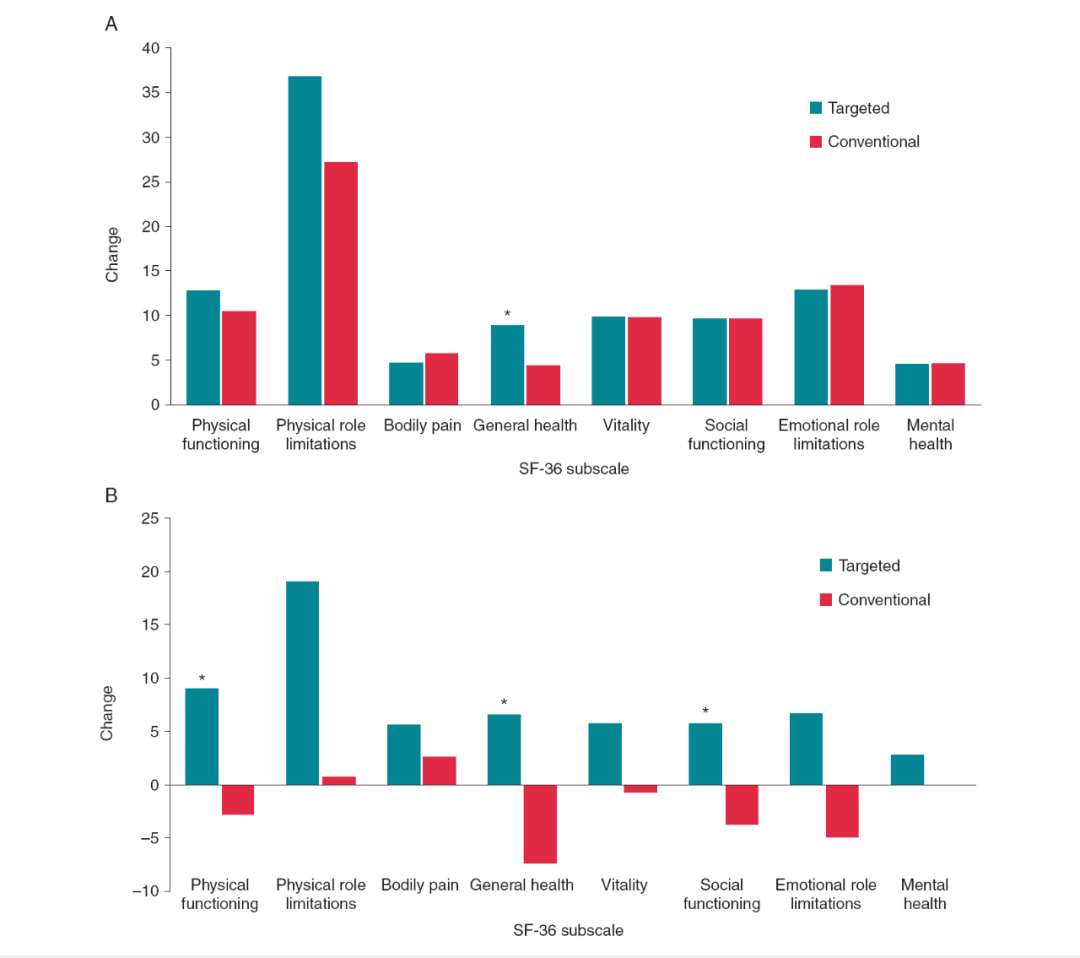
图片2019年在Europace上刊登的结果显示:与传统治疗相比,治疗早期持续性房颤和心衰的策略能更好地改善患者的生活质量。甚至在房颤患者1年时也观察到其益处。
Methods and results
常规与侵袭性危险因素驱动的上游心律控制预防心力衰竭早期房颤的比较研究(RACE 3)将早期持续性房颤和心衰患者随机分为靶向治疗和常规治疗。两组均接受指导性治疗。目标组接受四种额外的治疗:盐皮质激素受体拮抗剂;他汀类药物;血管紧张素转换酶抑制剂和/或受体阻滞剂;心脏康复,包括体力活动、饮食限制和咨询。对230名患者在基线检查时和1年后的生活质量进行分析,包括可用的医疗结果研究简式健康调查(SF-36)、多伦多大学房颤严重程度量表(AFSS)问卷和欧洲心律协会(EHRA)等级。SF-36子量表在目标组的身体功能(Δ12±19 vs.Δ6±22,P=0.007)、身体角色限制(Δ32±41 vs.Δ17±45,P=0.018)和一般健康(Δ8±16 vs.Δ0±17,P<0.001)方面的改善更大。静息呼吸困难改善更多(Δ?0.8?±?1.3 vs.Δ?0.4?±?1.2,P?=?0.018),目标组随访1年时EHRA分级更低。1岁时房颤患者,身体功能改善(Δ9±?9 vs.Δ?3±?16,P?=?0.001),一般健康(Δ7±?16 vs.Δ?7±?19,P?=?0.004)和社会功能改善(Δ6±?23 vs.Δ?4±?16,P?=?0.041)在目标组中较大。
Am Heart J
RACE 3 · 2020
图片2020年09月在Am Heart J上刊登的结果显示:研究结果再次强调,对持续性房颤和中度心衰患者进行心律控制治疗的早期治疗具有重要的潜力。
Results
共有194名患者被纳入本分析,其中119名患者中有68名(57%)为靶向患者和所有常规患者(N=126)。目标患者只有在符合所有最佳标准时才被纳入。在靶向组中,94例(79%)患者符合最佳血压标准,100例(84%)符合最佳低密度脂蛋白胆固醇标准,91例(76%)符合最佳NTproBNP标准。这导致119名患者中有68名(57%)符合所有最佳治疗标准。
1年时,优化组68例患者中有59例(87%)出现窦性心律,而常规组126例患者中有79例(63%)出现窦性心律(图1A)。使用盐皮质激素受体(64[94%]vs.5[4%];P b.001)、ACE抑制剂和ARBs(61[90%]vs.96[76%];P=0.049)以及他汀类药物(66[97%]vs.61[48%];P b.001)在1年时在优化组和常规组之间存在显着差异(图1B)。重复ECV的患者数(32[47%]比64[51%];P=0.654),前6个月ECV总数(35比75;P=0.486)和后6个月ECV总数(17比18;P=0.112),服用任何抗心律失常药物(31[46%]比54[43%];P=0.763),索他洛尔(11[16%]比16[13%];P=0.520),胺碘酮(17[25%]比31[25%];P=1.000),氟卡胺(9[13%}对9[7%];P=0.197)、决奈达隆(0[0%]对2[2%];P=0.542)以及心房消融(1[2%]对2[2%];P=1.000)的使用具有可比性。

Int J Cardiol Heart Vasc
RACE 3 · 2020

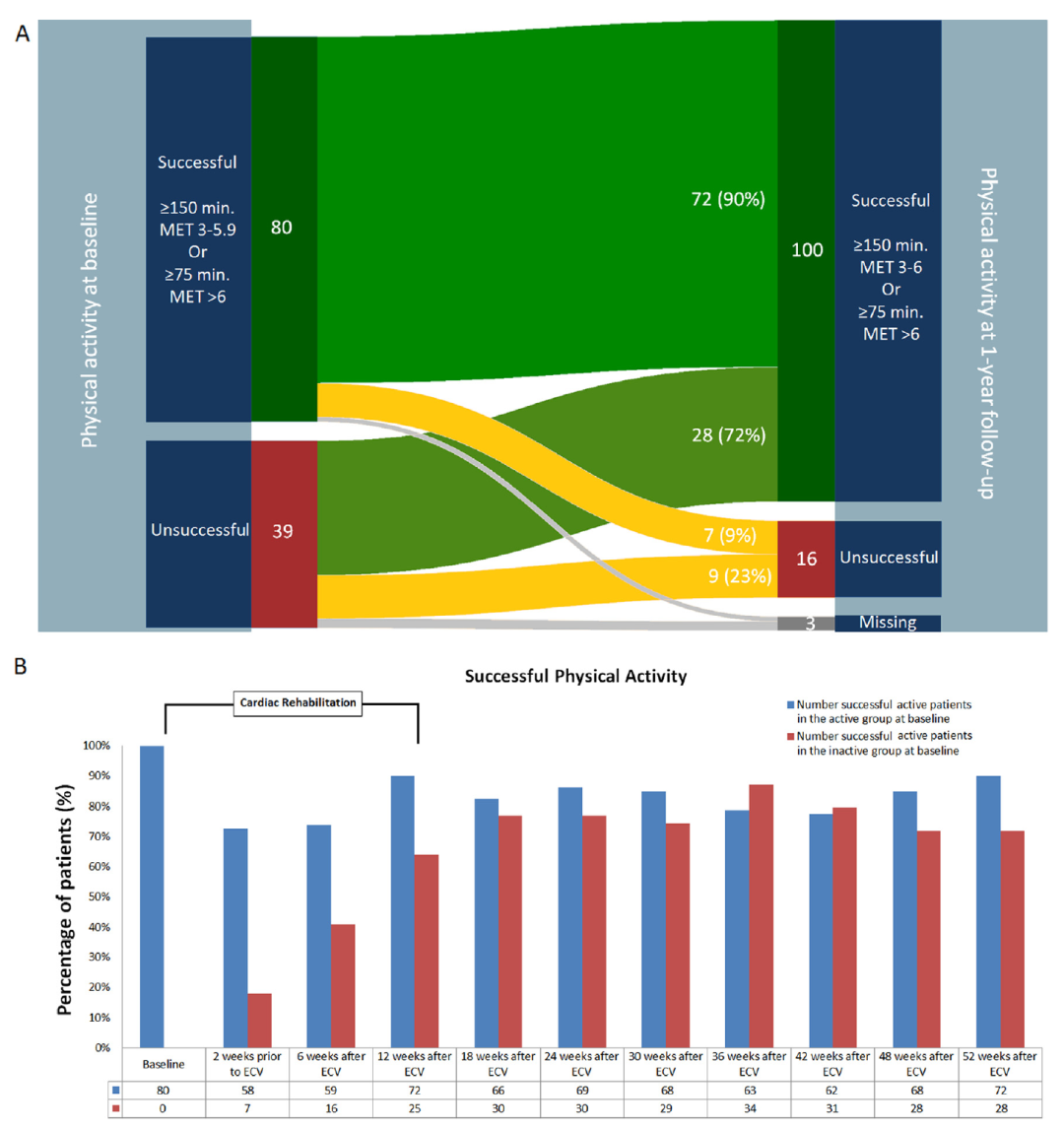
图片2020年11月在Int J Cardiol Heart Vasc上刊登的结果显示:对于持续性房颤和中度心力衰竭患者,参与心脏康复(CR)有助于改善和维持体力活动。
Results
目标组119例患者全部参加CR治疗,106例(89%)完成CR治疗。在基线检查时,80例(67%)患者成功地进行了体力活动,39例(33%)没有。活动期患者的NTproBNP较低。在1年的随访中,体力活动患者保持活跃:12周时72(90%),1年时72(90%)。不活跃的患者变得活跃:12周时25例(64%),1年时30例(77%)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#稳定型#
65
#长期结果#
57
#ACE#
63
#持续性#
84
#EHRA 2021#点击进入话题查看更多相关文章 或评论时插入话题加入讨论
111
好文章
95
#CTS#
104
#心房#
65
房颤,临床上碰到很多哦
80