Cancer Research:外泌体非编码RNA与肿瘤耐药
2020-07-22 A pioneer 免疫细胞研究bioworld
癌症是目前人类无法克服的问题。目前实体瘤的治疗主要有手术切除、化疗、靶向治疗和放疗,其中化疗在控制肿瘤进展中发挥着重要作用。由于化疗药物的耐药降低了治疗效果,肿瘤耐药一直是研究的重要课题。
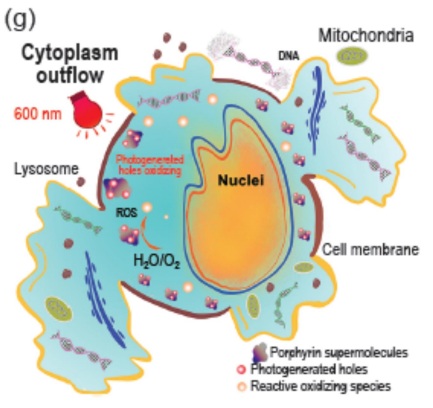
癌症是目前人类无法克服的问题。目前实体瘤的治疗主要有手术切除、化疗、靶向治疗和放疗,其中化疗在控制肿瘤进展中发挥着重要作用。由于化疗药物的耐药降低了治疗效果,肿瘤耐药一直是研究的重要课题。肿瘤耐药可能是由于基因或表型改变或肿瘤微环境(TME)阻止药物进入肿瘤细胞所致。研究表明,内皮细胞的外泌体在化学抗性中发挥作用。外泌体作为细胞间通讯的信号载体,通过转运蛋白、mRNA、免疫细胞和非编码RNA (ncRNA)参与耐药调控。NcRNAs包括microRNAs (miRNAs)、长链非编码rna (lncRNAs)和环状rna (circRNAs),近年来得到越来越多的研究。值得注意的是,最新研究表明,外泌体ncRNAs在肿瘤耐药中起着关键作用。例如,外泌体传输的miR-128-3p增加了奥沙利铂耐药结直肠癌(CRC)的化疗敏感性。研究人员还发现了许多外泌体ncRNA,它们可以增加或降低其他癌症的化学敏感性。外泌体ncRNA不仅影响化疗敏感性,而且还调节肿瘤耐药的发展和进展机制。
外泌体ncRNA调控耐药的机制多种多样。综述了外泌体ncRNA在药物外排、信号通路激活、药物靶点调控和TME修饰中的变化。作者还将讨论不同癌症中的外泌体ncRNA和解决耐药性的未来。外泌体来源ncRNAs的发现对肿瘤耐药具有诊断和预后价值。
1. 外泌体ncRNA的特征
细胞外囊泡已成为细胞间生理和病理生理交流的重要介质。EV可作为新的生物标志物用于多种疾病的治疗。当EV用于功能研究时,其分离纯度是非常重要的。目前,差速离心法、密度梯度离心法和尺寸排阻色谱法是研究人员最常用的纯化EV的方法。这些细胞源性膜结构由外泌体和微胶囊组成,前者来自核内体网络,后者来自质膜。外泌体是由细胞衍生的小脂泡,包含DNA, mRNA, ncRNA,脂质和蛋白质。最近大量研究表明,外泌体由多种细胞类型和细胞系分泌,包括肿瘤细胞、免疫细胞、成纤维细胞、脂肪细胞和神经元细胞。最近许多研究表明,外泌体可由多种细胞类型和细胞系分泌,包括肿瘤细胞、免疫细胞、成纤维细胞、脂肪细胞和神经细胞以及其他体液。外泌体是由内吞小泡出芽产生多泡状小体(MVBs)形成的,多泡状小体结合到质膜中,此时小泡状物质被释放。外泌体的形成涉及运输所需的内体分选复合体(ESCRT),它结合并将蛋白质分选到MVBs的腔内小泡中。ESCRT结合许多附件蛋白并识别泛素化蛋白。此外,不依赖ESCRT的机制也可以产生外泌体。
2. 癌症中的外泌体ncRNA
消化系统肿瘤(DSC)由CRC、胃癌、肝细胞癌、胰腺癌和食管鳞状细胞癌组成,是全球癌症相关死亡的主要原因之一。晚期DSC患者的低生存率不仅与肿瘤复发转移有关,还与耐药有关。NcRNAs在肿瘤中异常表达,在DSC耐药过程中发挥重要作用。对奥沙利铂耐药的晚期结直肠癌患者的治疗仍然不足。研究人员证实,与正常细胞和细胞系相比,CRC细胞和细胞系中miR-128-3p表达显着下调。Bmi1是miR-128-3p调控EMT的功能靶点。miR-128-3p降低导致Bmi1过表达,可能导致化疗诱导的CRC细胞EMT,进而触发奥沙利铂从CRC细胞外排,导致耐药。外泌体可能携带miR-128-3p并将其转移到受体细胞,从而阻止miR-128-3p的降解。在奥沙利铂耐药细胞中,外泌体miR-128-3p改变其靶基因Bmi1和MRP5的表达,从而恢复CRC细胞对化疗药物的敏感性。
吉西他滨(20,2 -二氟-2 -脱氧胞苷)仍然是胰腺癌患者的首选药物,可以单独使用,也可以与其他化疗药物联合使用。化疗药物产生活性氧是其细胞毒作用的重要机制之一。既往有研究报道,CAT和SOD2在一定程度上参与了胰腺癌的获得性耐药,并促进了多种癌症的化学耐药。外泌体miRNA转移到耐药肿瘤细胞抑制DCK(吉西他滨代谢基因),从而诱导吉西他滨耐药。MiR-155是新发现的调控胰腺癌DCK表达的因子。
来自M2极化巨噬细胞的外泌体被胃癌细胞吸收,因此外泌体可能携带miR-21从巨噬细胞进入胃癌细胞。因为miR-21降低化疗敏感性和凋亡,外泌体miR-21产生顺铂耐药。
总结
综上所述,外泌体ncRNAs在肿瘤耐药中的作用已逐渐被揭示。外泌体作为天然载体,转移ncRNA和参与耐药的蛋白质。本文综述了外泌体ncRNA在增加肿瘤药物外排、改变药物靶点、激活信号通路和调控TME中的生物学作用。本文还讨论了肿瘤靶向药物和外泌体ncRNA作为生物标志物的潜在治疗价值。研究人员发现,在不同的癌症中,ncRNA通过不同的途径调节肿瘤耐药。化疗耐药在癌症治疗中仍然是一个严重的问题,而外泌体ncRNA在这类治疗中的潜在作用尚不清楚。迄今为止,在细胞水平上将有希望的实验结果转化为临床试验仍然是最困难的挑战。因此,了解外泌体ncRNA在各种肿瘤中调控耐药性的机制,将有助于改善癌症治疗。
原始出处:
Chengyao Guo 1, Jinbo Liu 1, Quanbo Zhou 1, et al.Exosomal noncoding RNAs and tumor drug resistance.Cancer Res. 2020 Jul 8;canres.0032.2020. doi: 10.1158/0008-5472.CAN-20-0032.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#外泌体#与#肿瘤#的关系,未来会持续是热点。包括在肿瘤的诊断,转移,耐药,治疗反应性和预后的相关性
196
很有帮助
109
#非编码#
72
#Research#
51
#编码#
49
学习
114
了解一下
123