JACC子刊:新一代药物洗脱支架PCI后,女性更容易出现胸痛!
2016-03-30 Seven L MedSci原创
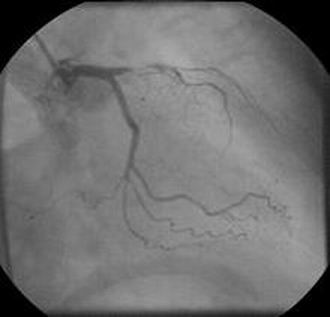
合并分析DUTCH PEERS和TWENTE随机试验后发现,使用新一代药物洗脱支架进行PCI的临床相关性胸痛的发生率具有性别差异,女性显著高于男性!合并分析研究共包括3202名稳定性或急性ACS患者,使用新一代永久性聚合物涂层的药物洗脱支架治疗。DUTCH PEERS试验中,患者随机分为Resolute佐他莫司洗脱支架 (Medtronic Vascular)或Xience V依维莫司洗脱支架(A
合并分析DUTCH PEERS和TWENTE随机试验后发现,使用新一代药物洗脱支架进行PCI的临床相关性胸痛的发生率具有性别差异,女性显著高于男性!
合并分析研究共包括3202名稳定性或急性ACS患者,使用新一代永久性聚合物涂层的药物洗脱支架治疗。DUTCH PEERS试验中,患者随机分为Resolute佐他莫司洗脱支架 (Medtronic Vascular)或Xience V依维莫司洗脱支架(Abbott Vascular)。TWENTE试验中,患者随机分为Resolute佐他莫司洗脱支架 (Medtronic Vascular)或Promus Element依维莫司洗脱支架(Boston Scientific)。
合并研究后,27%的患者为女性,与男性相比,女性年龄更大(平均 67.5岁 vs 62.8岁)、更多的CV危险因素:糖尿病(24.2% vs. 17.8%)、高血压(63.6% vs. 51.6%)、相关家族史(54.5% vs. 50.1%)。
研究人员对PCI术后第1年和第2年患者的胸痛情况进行了分析,数据来自于患者门诊或电话/医疗问卷调查随访。其中有99.8%的患者有临床随访数据,术后第1年和第2年胸痛发生率分别为94.1%和93.6%。
PCI术后第1年,患者自我报告的临床相关性胸痛的发生率在女性中更多见(16.3% vs. 10.5%; P < .001),第2年仍是女性患者胸痛情况更多见(17.2% vs. 11.1%; P < .001)。
多因素分析显示,“性别”是随访过程中临床相关性胸痛的独立预测因素。在PCI术后第2年,正常活动时,女性患者的胸痛风险增加1.8倍,休息时为1.7倍。
不过无论男女患者,在第2年,其心肌梗死死亡率、血运重建、支架血栓形成和复合终点的发生率是相似的。
研究者总结说:“虽然使用新一代药物洗脱支架进行PCI后,心血管不良事件发生率在男女患者见不存在差异,但是女性患者却比男性患者有显著更高的胸痛发生率,胸痛的发生可能是不同于冠状动脉阻塞的机制所致。”
原始出处:
Kok MM, et al.Sex Difference in Chest Pain After Implantation of Newer Generation Coronary Drug-Eluting Stents. J Am Coll Cardiol Intv. 2016;doi:10.1016/j.jcin.2015.10.043.
Women undergoing PCI with newer DES have higher prevalence of chest pain.Healio.March 29, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#洗脱支架#
66
#JACC#
72
#药物洗脱支架#
64
#ACC#
66