JAMA Surg:为何接受冠脉支架介入术与患者预后明显相关?
2016-01-01 QQduhp 译 MedSci原创
背景目前医生主要依据患者疾病原因推迟冠状动脉支架置入术。然而,防止支架的原因或许是导致民众出现术后主要不良心血管事件(MACE)的一个重要的风险因素。 目的该研究的目的是确定冠状动脉支架放置术指征是否为导致民众出现MACE的主要危险因素。 设计该研究为回顾性队列研究,参与人员均于2000.1.1-2010.12.31在美国退伍军人医院接受冠状动脉支架置入术,并在2年内接受非心脏手术。研究人员使用逻
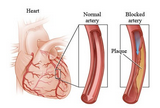
背景:目前医生主要依据患者疾病原因推迟冠状动脉支架置入术。然而,防止支架的原因或许是导致民众出现术后主要不良心血管事件(MACE)的一个重要的风险因素。
目的:该研究的目的是确定冠状动脉支架放置术指征是否为导致民众出现MACE的主要危险因素。
设计:该研究为回顾性队列研究,参与人员均于2000.1.1-2010.12.31在美国退伍军人医院接受冠状动脉支架置入术,并在2年内接受非心脏手术。研究人员使用逻辑回归模型来分析参与人员支架与术后MACE发生率之间的关系,并控制了相关因素。接受冠状动脉支架置入术的三个指征为:(1)心肌梗死(MI);(2)不稳定性心绞痛;(3)与急性冠脉综合征无关的血管再生(非ACS)。
研究人员关注的主要结果为术后30天内患者出现MACE(包括MI和血管再生)的发生率及病人的全因死亡率。
结果:在26661名平均年龄为68岁的患者(年龄范围为(61.0——76.0)中,98.4%为男性,88.1%为白人)接受冠状动脉支架置入术后2年内接受了41815例手术。其中,32.8%的患者因心肌梗死而接受手术,33.8%的患者因不稳定性心绞痛接受手术,33.4%的患者因与急性冠脉综合征无关的血管再生而接受手术。因MI接受手术的患者发生MACE的发生率(7.5%)明显高于后两组患者(不稳定心绞痛:2.7%,血管再生:2.6%,P <0.001)。对于接受经皮冠状动脉介入术3个月内的患者而言,MI组调整后优势比明显高于非ACS组优势比(OR=5.25;95%CI:4.08——6.75)。随着时间的推移,这种风险比例降低,但是在接受经皮冠状动脉介入后1-2年内MI组风险仍较高(OR = 1.95;95%CI:1.95——1.58)。术后3个月内及1-2年内不稳定性心绞痛组患者的调整后风险比与血管再生组相似(OR = 1.11,95% CI,:0.80-1.53;OR = 1.08,95% CI: 0.86-1.37)。支架类型与MACE发生率无明显关联。
结论:研究表明,相比而言,因心肌梗死接受冠状动脉支架放置术的患者术后MACE发生率远高于其他原因接受冠脉支架放置术的患者。不论支架类型如何,随着时间的推移,PCI术后MACE发生率降低。
原始出处:
Carla N. Holcomb,Robert H. Hollis,et al.Association of Coronary Stent Indication With Postoperative Outcomes Following Noncardiac Surgery.JAMA Surg.December 30, 2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#冠脉支架#
92
#患者预后#
81
十年的大样本研究,不错的文章
169
值得关注
203
好文
163
赞
160
不错的文章哦,多看
170
不错的文章,
100
哦,
41
嗯,
180