JAMA Neurol :傻傻分不清楚……看起来是帕金森病,其实是罕见神经退行性疾病?
2020-11-12 探索菌 生物探索
神经元核内包涵体病(NIID)是近年来新发现的一类罕见神经退行性疾病,有证据表明,NOTCH2NLC基因中GGC异常重复扩增与NIID有关,但目前尚无有效的治疗方法。
神经元核内包涵体病(NIID)是近年来新发现的一类罕见神经退行性疾病,有证据表明,NOTCH2NLC基因中GGC异常重复扩增与NIID有关,但目前尚无有效的治疗方法。NIID的症状包括痴呆、帕金森病、平衡不佳以及四肢麻木和无力。NIID患者可能会出现相应症状,也可能不会,具体取决于年龄和疾病阶段。然而,尚未表明NOTCH2NLC GGC重复序列与帕金森病(PD)之间是否存在关联。
最近,新加坡国家神经科学研究所和新加坡总医院的一项联合研究表明,被诊断患有PD的患者实际上可能患有NIID。相关研究成果发表于《JAMA Neurology》上。
该团队在十多年里共招募了2076名参与者,包括1000名PD患者和1076名健康参与者。对他们的NOTCH2NLC GGC重复扩增进行基因筛查后发现,被诊断为PD的患者出现了会导致NIID的突变。共有13例PD患者携带的NOTCH2NLC GGC重复扩增大于40个单位,有2名PD患者甚至出现了122和79个重复序列,而临床NIID病例的重复扩增有65次以上。
本研究第一作者Ma Dongrui博士表示:“据我们所知,这是第一项报道PD患者携带NOTCH2NLC基因突变的研究,就如同在NIID患者中观察到的那样。幸运的是,这些患者对PD药物的反应要比大多数PD患者更好,这表明一定有某些因素导致了某些人会发展为PD而另一些人会发展为更严重的NIID。
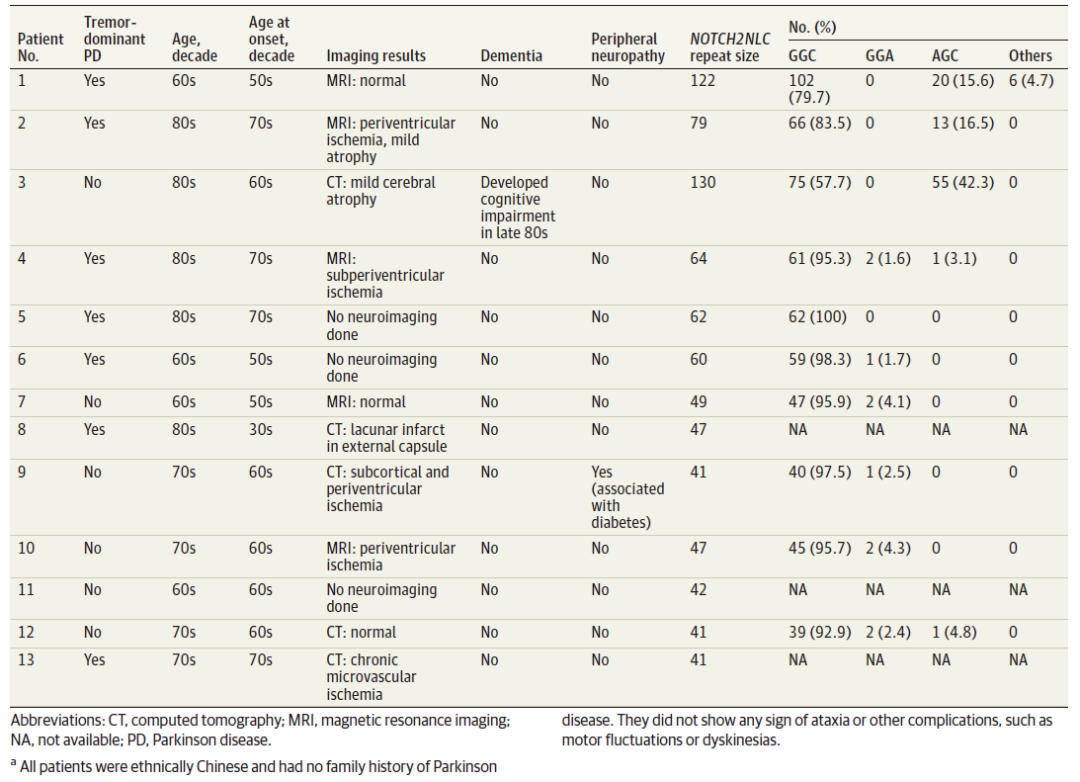
帕金森病和NOTCH2NLC重复扩展大于40a的患者的临床特征
此外,研究小组还发现,有些PD患者的NOTCH2NLC GGC基因出现了轻微重复扩增(扩增次数为40至64),虽然扩增次数没有超过65,但重复范围的致病性仍需进一步研究。41至64个重复序列的扩增可能构成PD的遗传风险或代表不同的关联,但这是否代表具有随后临床表现潜力的内表型仍是一个推测。
由于NIID可能无法被检测到,因此PD患者是否患有NIID需要高度怀疑。利用目前所知道的信息,临床医生注意早期的认知障碍或影像学证据可能会提示诊断为PD的患者存在NIID。研究人员也建议,由于NIID是由基因突变引起的,因此也有必要寻找可能显示出NIID症状的PD患者的家庭成员。
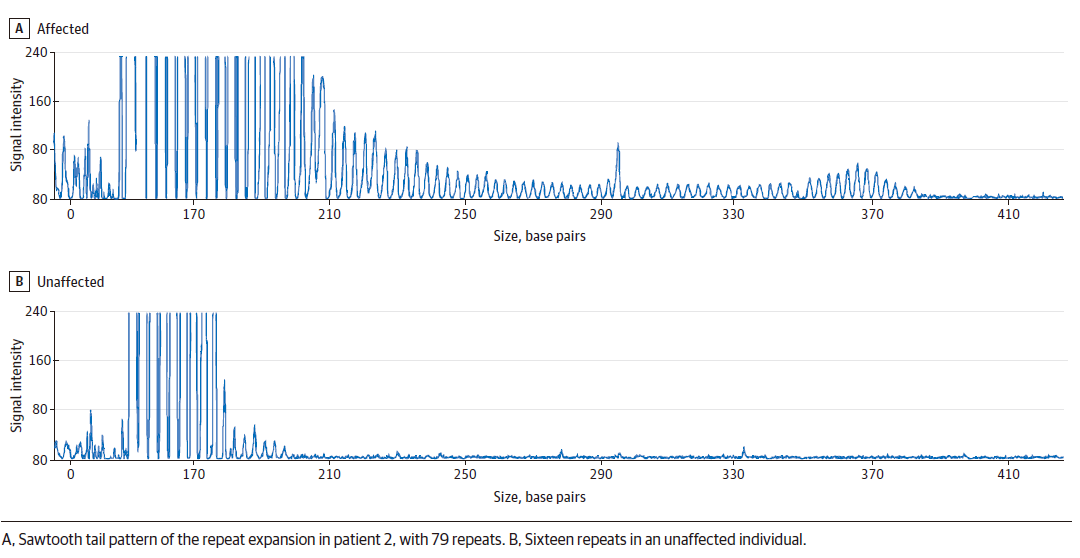
重复灌注聚合酶链反应的代表性电泳图显示了异常的NOTCH2NLC GGC重复扩展
未来,研究小组计划进行更多的研究来了解NIID背后的机制,并找到针对这种情况的新药。NIID的广泛临床表型是否与NOTCH2NLC基因位点、种族或其他因素的微妙遗传差异有关,还需要深入研究来。不过,对具有PD表型的基因突变携带者的长期随访可能会提供其他线索。
总之,这项研究结果表明,许多神经退行性疾病重叠且可能具有共同的病因。找到共同的联系并揭示为何相似的基因突变却导致了两种疾病(轻度PD和严重NIID)的原因,有助于寻找针对这些疾病的新药。
原始出处:
Dongrui Ma, Yi Jayne Tan, Adeline S L Ng, et al.Association of NOTCH2NLC Repeat Expansions With Parkinson Disease.JAMA Neurol. 2020 Aug 24;e203023. doi: 10.1001/jamaneurol.2020.3023.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#退行性疾病#
96
#神经退行#
79
#Neurol#
79
涨知识了
123
NIID这几年在国内火的,不算少见了😂
120
#罕见#
81
还能这个样子…学习到了学习到了
132
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
88