JACC:酒精滥用危害等同于高血压和糖尿病,增2倍房颤、1.4倍心梗和2.3倍心衰风险
2017-01-04 卢芳 中国循环杂志
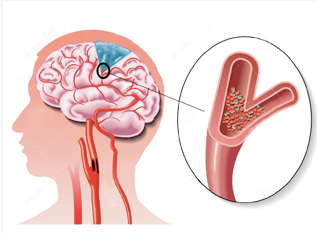
酒,已经深深地印在全球人民的生活中了。但近日发表于JACC上的一项研究表明,酒精滥用等同高血压、糖尿病、吸烟、肥胖等已经明确的心血管危险因素,可以增加房颤、心梗和充血性心衰等发生风险。 这是研究者对美国加州2005-2009年1470万门诊外科、急诊和住院患者进行分析的结果。其中有1.8%的受试者有明确的酒精滥用诊断。酒精滥用,并非酒精依赖,不过也是酒精使用障碍中一类疾病诊断,在“国际疾
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#滥用#
67
#JACC#
73
#ACC#
71
#心衰风险#
65
要戒酒了
120