JAHA:孤立性收缩压或舒张压高血压年轻人慢性肾脏病风险分析
2021-04-01 MedSci原创 MedSci原创
在血压升高、1期IDH、、1期ISH、1期SDH、2期IDH、2期ISH和2期SDH的参与者发生CKD风险高于正常BP参与者。ISH和IDH组的CKD风险相似,但低于SDH组。
年轻人中高血压疾病很常见。但是,尚不清楚年轻人中孤立性收缩压高血压(ISH)、孤立性舒张压高血压(IDH)或收缩压和舒张压高血压(SDH)对慢性肾脏疾病(CKD)发生的影响。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员纳入了2009年至2010年期间接受基础评估时未服用降压药且年龄在20至39岁之间的3030884名参与者。
参与者分类为血压正常、血压升高、1期IDH、1期ISH、1期SDH、2期IDH、2期ISH和2期SDH。该研究的主要结局是CKD事件。
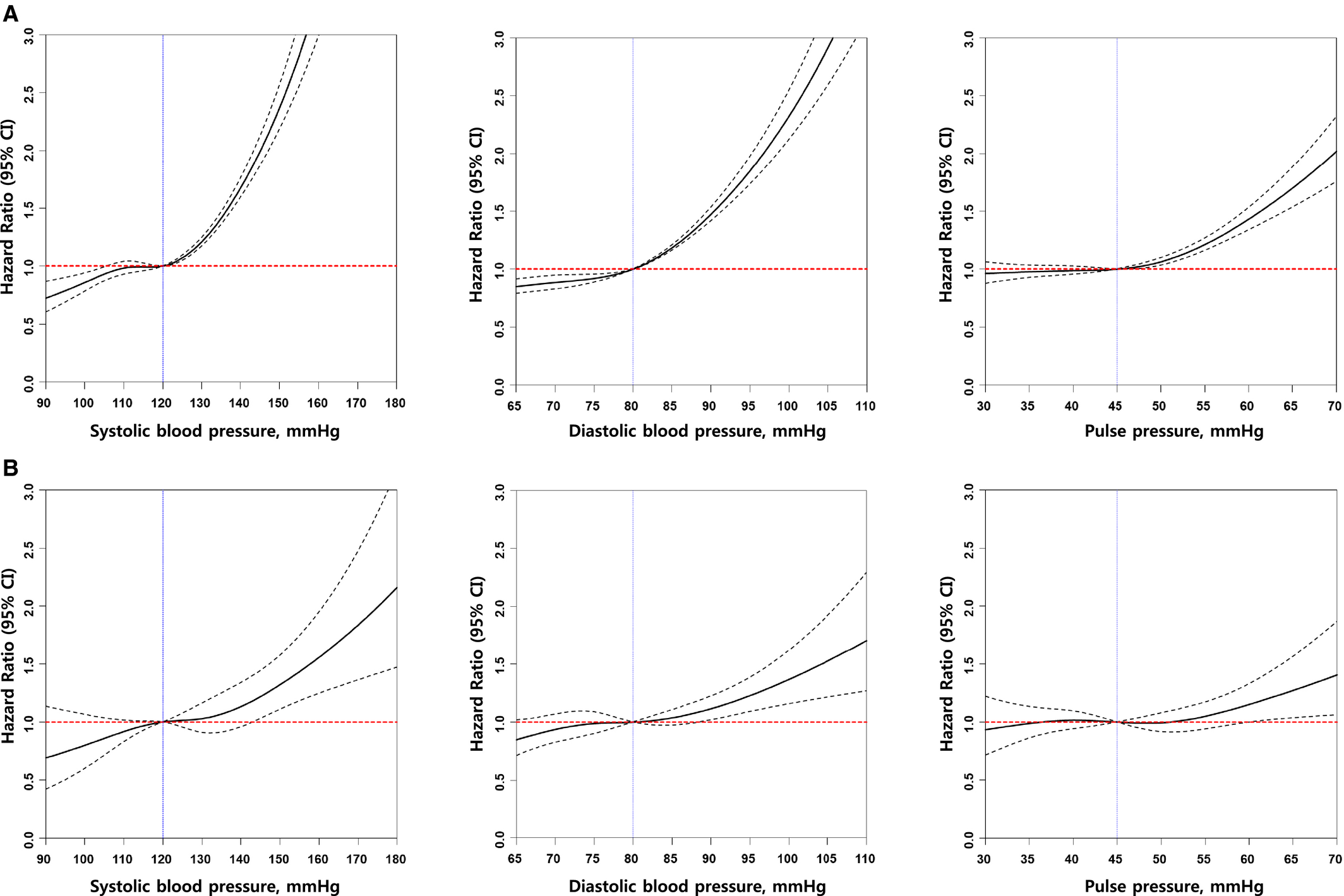
该研究总共发生了5853(0.19%)例CKD事件。以正常血压为对照,血压升高参与者CKD的多变量调整风险比(HRs)(95%CI)为1.14(95%CI为1.04-1.26),1期IDH患者为1.19(95%CI为1.10–1.28);1期ISH患者为1.24(95%CI为1.08–1.42);1期SDH患者为1.39(95%CI为1.28–1.51);2期IDH患者为1.88(95%CI为1.63-2.16);2期ISH患者为1.84(95%CI为1.54–2.19);2期SDH患者为2.70(95%CI为2.44–2.98)。在体检后1年内开始接受降压治疗的患者发生CKD的HRs较未接受降压治疗患者的HRs有所降低。
由此可见,在血压升高、1期IDH、、1期ISH、1期SDH、2期IDH、2期ISH和2期SDH的参与者发生CKD风险高于正常BP参与者。ISH和IDH组的CKD风险相似,但低于SDH组。降压药可减轻年轻高血压成年人的CKD风险。
原始出处:
Eun Hui Bae.et al.Chronic Kidney Disease Risk of Isolated Systolic or Diastolic Hypertension in Young Adults: A Nationwide Sample Based‐Cohort Study.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.019764
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#收缩压#
39
#AHA#
45
#舒张压#
45
#孤立性#
55
#慢性肾脏#
44
好
85