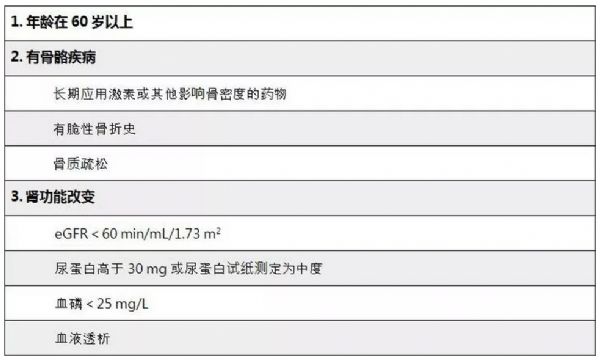
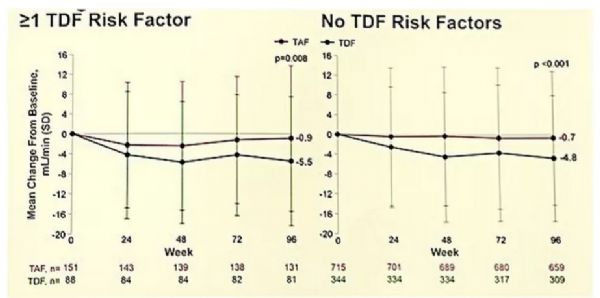
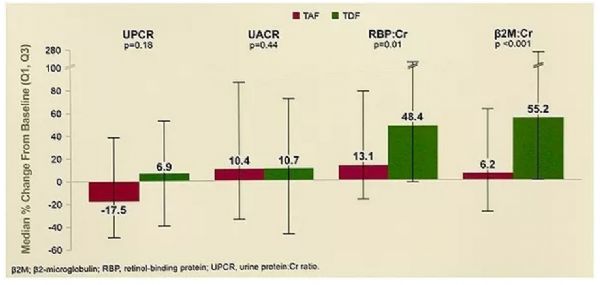
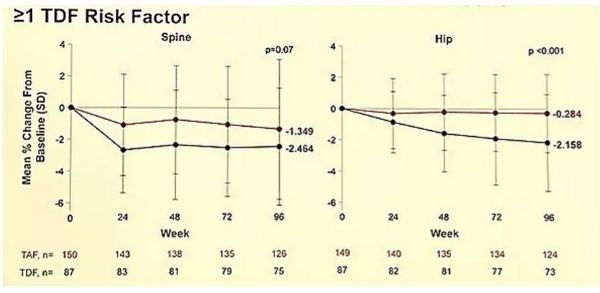
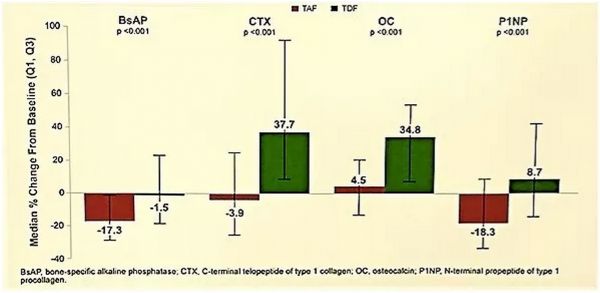
AASLD2017:有TDF基线风险因素的慢乙肝初治患者应用TAF的疗效和安全性分析
2017-10-29 佚名 国际肝病
随着慢乙肝患者的老龄化,患者用药的安全性越来越受到重视。目前恩替卡韦(ETV)、富马酸替诺福韦二吡呋酯(TDF)和磷丙替诺福韦(TAF)为EASL最新指南推荐的初治慢乙肝一线首选核苷(酸)类似物(NA)。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#疗效和安全性#
88
#TDF#
92
#AASLD#
67
#ASL#
66
非常好的文章.学习了
78
学习了受益匪浅
82
^_^^_^^_^
81
不错的分享
83