Mov Disord-新型标记物: 鞘氨醇-1-磷酸酯可预测帕金森的病情进展
2021-08-05 Freeman MedSci原创
新型标记物: 鞘氨醇-1-磷酸酯可预测帕金森的病情进展
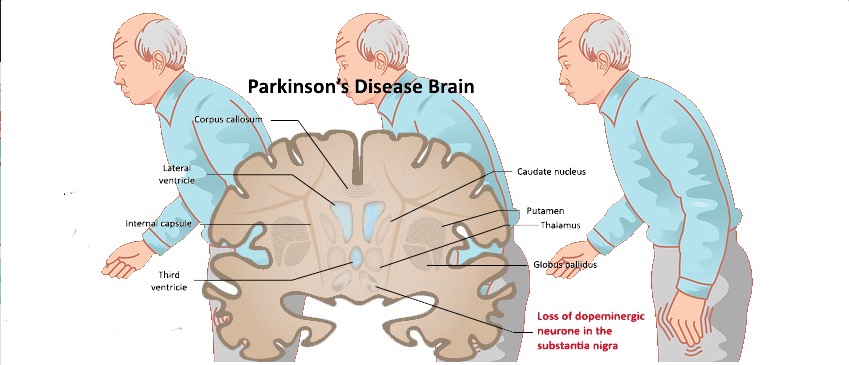
帕金森病(PD)是一种神经退行性疾病,具有多方面的潜在机制。在实验研究中,线粒体功能障碍、氧化应激增加、炎症、突触核蛋白聚集,以及最终的神经元死亡都与帕金森病的病理生理学有关。在帕金森病小鼠模型中,所有这些过程都可由鞘氨醇-1-磷酸(S1P)模拟物减弱。
在细胞培养实验中,S1P通过激活S1P受体1(S1PR1)信号和增强线粒体生物生成,保护多巴胺能神经元免受1-甲基-4-苯基-4-丙酸(MPP)诱发的细胞死亡。
除了体外实验,S1P受体调节剂芬戈里莫德(fingolimod)减少了α-突触蛋白的聚集,增加了脑源性神经营养因子(BDNF),减弱了多巴胺能神经变性,减轻了纹状体多巴胺水平的下降,并最终减少了不同药物诱导的PD小鼠模型的运动障碍。芬戈里莫德在这些PD小鼠模型中的有益作用被归因于S1PR1的激活,因为选择性的S1PR1拮抗剂阻断了芬戈里莫德的神经保护作用。
虽然大多数研究都集中在芬戈里莫德对自身免疫性疾病的免疫调节作用上,但S1P在脑血管功能方面也发挥着重要作用。最重要的是,S1P信号对脑内皮细胞维持适当的紧密连接功能,进而维持完整的血脑屏障是强制性的。因此,S1P在亨廷顿氏症和阿尔茨海默氏症的小鼠模型中也赋予神经保护作用。
尽管体外和体内的实验研究表明,S1P在PD模型中具有神经保护作用,但尚未研究血清S1P水平与PD及其表型之间的关系。
藉此,德国汉堡大学的Edzard Schwedhelm等人,探究了S1P在PD患者中,和运动和认知功能的关系。
他们使用液相色谱-串联质谱法(LC-MS/MS)分析了196名帕金森病患者和196名年龄和性别匹配的对照组的血清中的S1P浓度。在基线时评估了运动(及运输帕金森病评分表III[UPDRS III],Hoehn和Yahr)和认知功能(基于蒙特利尔认知评估量表[MoCA])。有64名患者的随访数据(中位随访513天)。
 他们发现:与对照组相比,PD患者的S1P水平较低,分别为1.75(1.38-2.07)和1.90(1.59-2.18)μmol/L (P = 0.001)。
他们发现:与对照组相比,PD患者的S1P水平较低,分别为1.75(1.38-2.07)和1.90(1.59-2.18)μmol/L (P = 0.001)。
在PD患者中,较低的S1P浓度与较高的UPDRS III评分和Hoehn和Yahr阶段有关。
在随访队列中,低于中位数的分组中,,S1P浓度与运动能力下降的速度有关(HR=4.78 [95% CI, 1.98, 11.50]),但与认知能力的恶化无关。
这个研究的重要意义在于发现了:S1P功能有效预测PD患者的运动能力,及其进展。
原文出处:
Schwedhelm E, Englisch C, Niemann L, et al. Sphingosine‐1‐Phosphate, Motor Severity, and Progression in Parkinson’s Disease ( MARK‐PD ). _Mov Disord_. May 2021:mds.28652. doi:10.1002/mds.28652.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Disord#
69
#Dis#
62
#病情#
77
#标记物#
75