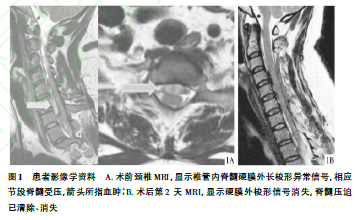
急性自发性硬脊膜外血肿漏诊1例
2019-10-30 向定朝 马传雨 临床骨科杂志
患者,女,41岁,2016年9月18日凌晨2点左右出现颈后酸胀、疼痛不适,睡眠中痛醒,至我院急诊科就诊。考虑颈椎疾病,行颈椎X线检查未见明显异常;建议患者行颈椎MRI检查并留院观察,因患者及家属拒绝,故予颈托外固定、镇痛治疗,患者好转后自行回家。当日上午9点30分,患者感颈后仍疼痛难忍,再次至骨科门诊就诊。查体:神志清,精神一般,痛苦面貌,颈后叩痛、压痛,颈椎屈伸、旋转功能受限,双手霍夫曼征阴性,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#血肿#
76
#漏诊#
82
#硬脊膜#
73
#自发性#
86