Orbit:基于CT体积测量研究眶前和眶内软组织体积与眼眶爆裂性骨折的风险的相关性
2018-08-22 cuiguizhong MedSci原创
华盛顿大学眼科及阿拉巴马大学伯明翰分校眼科的Jacobs SM近日在Orbit杂志上发表了一项重要的工作。眼眶爆裂性骨折一般是由创伤造成的,在保留边缘的同时打破了眶壁。以前对骨折机制的研究主要集中在骨骼解剖学上。本研究评估了眶前和眶内软组织体积在骨折风险中的作用。
华盛顿大学眼科及阿拉巴马大学伯明翰分校眼科的Jacobs SM近日在Orbit杂志上发表了一项重要的工作。眼眶爆裂性骨折一般是由创伤造成的,在保留边缘的同时打破了眶壁。以前对骨折机制的研究主要集中在骨骼解剖学上。本研究评估了眶前和眶内软组织体积在骨折风险中的作用。

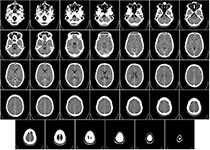
他们对51例单侧眼眶爆裂性骨折患者进行了一项回顾性病例对照研究。通过可比较的机制,对照组进行眼眶创伤而不会发生骨折。通过计算机断层扫描(CT)图像对眼眶进行轴向上的细切处理,并在3D处理工作站上评估这些结果,以测量眼眶前和眼眶内的软组织体积,然后使用Mann-Whitney U分析两组之间差异。
在实验组中,有40名男性(78%)是由于受到攻击(66%)、跌倒(12%)、机动车碰撞(10%)或其他原因(12%)而造成的伤害。对照组中有33名男性(65%)是由于受伤(55%)、跌倒(22%)、机动车(4%)或其他原因(20%)而造成的伤害。病例组和对照组的机率无明显差异。病例组的中位前眶体积为12.5 cm3,对照组为14.1 cm3(p = 0.02)。病例组的眶内中位数体积为24.4 cm3,对照组为25.9 cm3(p = 0.003)。
CT容积分析显示,持续爆裂性骨折的患者眶前和眶内软组织容量低于未骨折的患者。这强调了软组织在消除眶缘前方和眼眶内部的冲击力等方面所起的重要作用。
原文出处:
Jacobs, S.M., et al., Association between pre- and intraorbital soft tissue volumes and the risk of orbital blowout fractures using CT-based volumetric measurements. Orbit, 2018: p. 1-5.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#眼眶爆裂性骨折#
65
#相关性#
60
#软组织#
66
#眼眶#
76
学习了,谢谢分享
98
学习了
103
学习了,谢谢分享。
89