J Rheumatol:与巨细胞动脉炎复发和糖皮质激素依赖相关的因素
2019-08-27 xiangting MedSci原创
LVV是复发和GC依赖的独立预测因子。需要进一步的前瞻性研究来证实这些发现,并确定LVV患者是否需要不同的治疗方法。
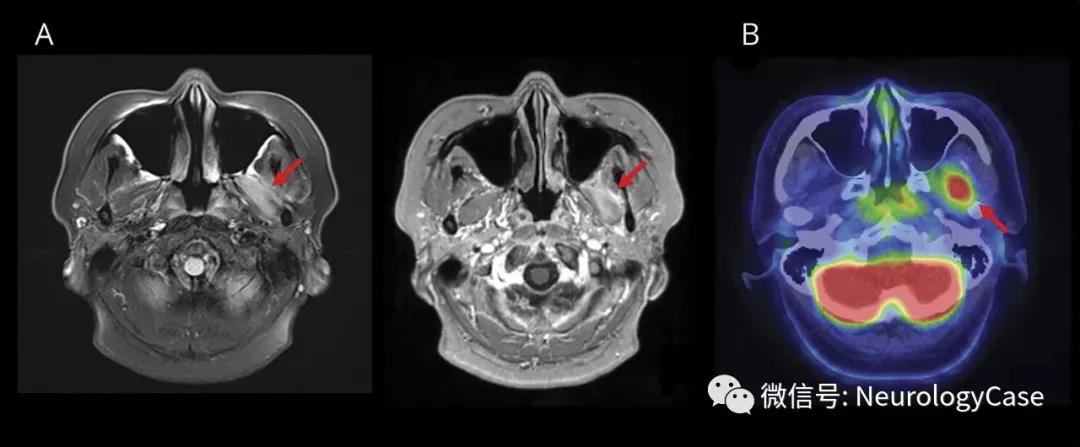
这项研究旨在确定巨细胞动脉炎(GCA)患者复发和糖皮质激素(GC)依赖的特征及相关因素。
研究回顾性分析了326例连续性GCA患者,随访至少12个月。在多因素分析中确定了与复发和GC依赖相关的因素。
对326例患者(73%为女性)进行了62个月的随访(12-262)。随访期间,171例患者(52%)复发,其中113例患者(35%)发生GC依赖。复发患者较少有卒中史(p=0.01),并且成像时大血管血管炎(LVV)比无复发患者更常见(p=0.01)。最初几个月,复发和非复发患者的治疗策略没有差别。与无GC依赖性疾病的患者相比,GC依赖患者的卒中史更少见(p=0.004),并且成像时的LVV更常见(p=0.005)。在多因素分析中,LVV是复发(HR 1.49,95%CI 1.002-2.12; p=0.04)和GC依赖的独立预测因子(OR 2.19,95%CI 1.19-4.05;p=0.01)。与之相反,卒中是复发(HR 0.21,95%CI 0.03-0.68; p=0.005)和GC依赖性疾病的保护性因素(OR 0.10,95%CI 0.001-0.31; p=0.0005)。接受GC保留剂治疗的GC依赖患者的GC治疗时间短于没有使用保留剂的患者(p=0.008)。
在这项研究中,LVV是复发和GC依赖的独立预测因子。需要进一步的前瞻性研究来证实这些发现,并确定LVV患者是否需要不同的治疗方法。
原始出处:
Anael Dumont. Factors Associated with Relapse and Dependence on Glucocorticoids in Giant Cell. J Rheumatol. 15 August 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#糖皮质#
53
#动脉炎#
54
#巨细胞#
53
#皮质激素#
44
学习了,学习了
103
学习了,谢谢分享
77
好
91