SCI REP:合成生物视网膜,这位牛津大学在读女博士很“拼”
2017-05-06 Flora 生物探索
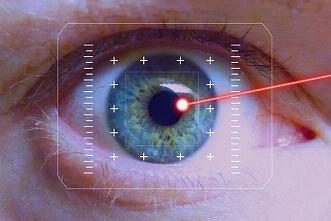
Vanessa Restrepo-Schild是一名就读于牛津大学化学系的理科博士生。年仅24岁的她带领团队合成出世界首个柔软的生物双层视网膜组织。这一研究有望彻底改变仿生植入产业,促成新的微创技术,从而帮助退行性眼疾的治疗,例如视网膜色素变性。相关研究成果发表在《Scientific Reports》期刊,Restrepo-Schild是文章的一作。视网膜位于眼球壁的内层,是一层透明的薄膜,专门

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#女博士#
71
#视网膜#
66
#牛津大学#
55
太好了,越来越深入了
79
学习了很有用
104