Sci Signal:维生素C的新功能-预防小胶质细胞激活
2017-03-29 xing.T MedSci原创
总体而言,该研究的结果表明抗坏血酸转运系统对于维持小胶质细胞动态平衡的重要性,以及提示抗坏血酸转运失调可能参与了神经系统疾病的发生发展。
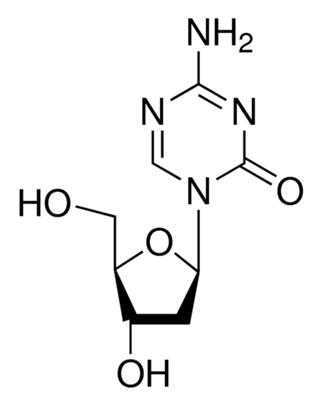
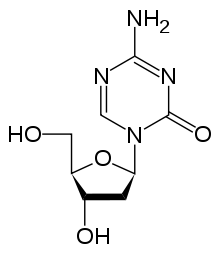
在中枢神经系统(CNS)中,维生素C的减少可以改变神经功能,并与神经发育和神经退行性疾病有关。由此可见,维生素C对于中枢神经系统的发育和功能是必不可少的。小胶质细胞的活化,在组织损伤或病原体入侵时发生的反应,也有助于神经退行性疾病的发生发展。细胞膜钠-维生素C协同转运蛋白2(SVCT2)是神经元摄取维生素C的主要介质。SVCT2特异性地转运抗坏血酸,维生素C的简化形式,作为还原剂。
近日,Science Signaling杂志上发表了一篇研究文章,研究人员的研究数据表明通过SVCT2吸收的抗坏血在维持小胶质细胞稳态中发挥着关键作用,小胶质细胞是位于CNS中的髓细胞,它对神经组织的正常运作是必不可少的。研究人员发现将SVCT2从细胞膜上敲除可以触发小胶质细胞的炎症表型,导致小胶质细胞的激活。Src介导了小胶质细胞caveolin-1蛋白tyr14位点磷酸化,诱导SVCT2蛋白内化。采用抗坏血酸治疗、SVCT2过表达或阻断SVCT2内化可以阻止小胶质细胞的激活。
总体而言,该研究的结果表明抗坏血酸转运系统对于维持小胶质细胞动态平衡的重要性,以及提示抗坏血酸转运失调可能参与了神经系统疾病的发生发展。
原始出处:
Camila C. Portugal, et al. Caveolin-1–mediated internalization of the vitamin C transporter SVCT2 in microglia triggers an inflammatory phenotype. Science Signaling. 2017. http://stke.sciencemag.org/content/10/472/eaal2005
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Signal#
95
#新功能#
89
#Sign#
77
#胶质细胞#
66
厉害了,我的哥
89
学习了,值得分享
114
学习了,维生素C非常重要
82
看看了解一下
110
好。。。。。
123