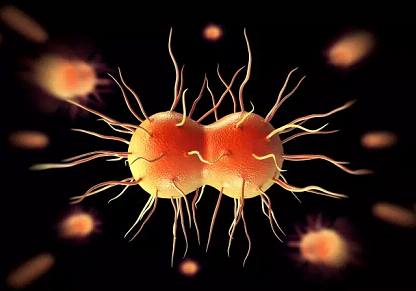
Clin Infect Dis:我国无并发症淋病头孢曲松钠治疗现状及治疗效果的研究结果
2019-04-21 不详 中国医学科学院
中国医学科学院皮肤病医院尹跃平研究员团队近期在《Clinical Infectious Diseases》杂志上发表了题为《Widespread Use of High-dose Ceftriaxone Therapy for Uncomplicated Gonorrhea Without Reported Ceftriaxone Treatment Failure: Results From 5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#治疗效果#
109
#头孢曲松钠#
84
#Dis#
100
#并发#
136
#研究结果#
90
#治疗现状#
69
#头孢曲松#
77
#头孢#
64
谢谢梅斯提供这么好的信息,学到很多
81
疗效只是效果的众多方面之一,还要看对患者的获益,包括生活质量等因素共同决定效果的
84