JAMA Neurology:他汀类药物预防阿尔兹海默病?服用2年降低15%的患病率
2016-12-15 生物探索 生物探索
导读 他汀类药物能够预防阿尔兹海默症?近期,《JAMA Neurology》期刊最新刊出一篇学术文章揭示,他汀类药物能够对大脑产生积极的影响,连续服用2年能够显著降低老年人患老年痴呆症的概率。
导读 他汀类药物能够预防阿尔兹海默症?近期,JAMA Neurology期刊最新刊出一篇学术文章揭示,他汀类药物能够对大脑产生积极的影响,连续服用2年能够显著降低老年人患老年痴呆症的概率。
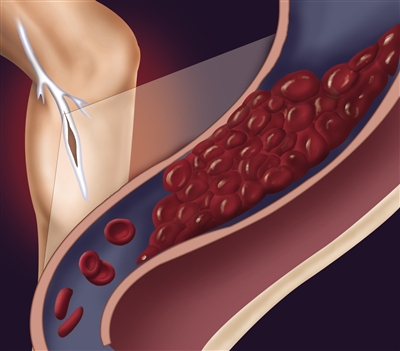
他汀类药物是降脂类降胆固醇、高脂血症领域的典型药物,其减缓动脉粥硬化的功效奠定了其在心血管疾病治疗中的重要地位。
来自于南加州大学的研究团队近期,发现除了心血管疾病,他汀类药物还有望应用于预防阿尔兹海默症。他们耗时7年(从2006年至2013年),对40万名美国老年人(65岁以上)进行调研分析。结果显示,他汀类药物能够对大脑产生积极的影响,女性服用这一廉价药物能够降低15%的患病率,男性能够降低12%。
Julie Zissimopoulos教授带领团队分析了调研对象是否服用他汀类药物、服用规律以及阿尔兹海默症患病等数据。总体而言,他们发现,每年会有1.72%的女性和1.32%的男性被确诊为阿尔兹海默症患者。但是,他汀类药物却鞥能够显著降低这一风险,且随着服药时间的延长,患病风险会进一步下降。
研究人员推测,胆固醇可能参与了淀粉样蛋白病斑的形成过程,而他汀类药物能够清理胆固醇,这有利于血液流向大脑,从而有助于抵制神经细胞的死亡。
他们发现,不同类型的他汀类药物对不同性别、种族的人有着不同的治疗效果,例如辛伐他汀(Simvastatin)会降低白人、西班牙裔和黑人女性以及白人、西班牙裔男性患痴呆症的风险。但是,对于黑人男性而言,任何类型的他汀类药物在预防痴呆风险上都没有显著差异。
Julie Zissimopoulos表示:“尽管经历了多年的研究,科学家们仍未研发出能够延缓甚至于逆转老年痴呆的药物。现在,这一最新数据意味着我们或许已经触摸到一个有效治疗手段,他汀类药物可以作为候选药物,用于降低阿尔兹海默症的风险。”
阿尔兹海默症协会研究主任Doug Brown博士评价这一最新研究表示:“”如此庞大的数据足以表明他汀类药物与老年痴呆症的关联性。但是,现有的数据并没有提供直接的证据,表明他汀类药物确实能够影响老年痴呆风险,这一结论仍然需要临床试验证实。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Neurol#
78
#他汀类药#
70
#患病率#
71
#阿尔兹海默#
80
#药物预防#
94