帕金森病(PD)是最常见的神经退行性疾病之一,其特点是具有广泛的临床表现。帕金森病的病理特征是α-synuclein(α-syn)在黑质中的不正常聚集。PD是一种高度异质性的疾病,临床症状和疾病进展因人而异。以前的研究已经确定了PD进展的几个预测因素,包括临床特征、脑脊液(CSF)生物标志物和遗传因素。然而,脂蛋白E(APOE)ε4与帕金森病患者运动进展的关系仍然未知。
APOE ε4等位基因是晚期阿尔茨海默病(AD)的最强风险因素,已知它与淀粉样β(Aβ)病理有关。以前的研究报告称,APOE ε4有助于PD痴呆的早发,但显示与PD发展的风险没有关联。令人惊讶的是,最近的证据表明,APOE ε4可以影响α-syn病理,而没有Aβ参与突触蛋白病的小鼠模型。此外,一项关于路易体(LB)疾病的死后研究表明,APOE ε4与弥漫性LB病理学有关,但与AD病理学无关,这表明APOE ε4可能直接导致PD的α-syn病理学。
藉此,浙江大学的Jia-Li Pu等人,利用PPMI队列探讨APOE ε4是否对PD患者的疾病进展有贡献。
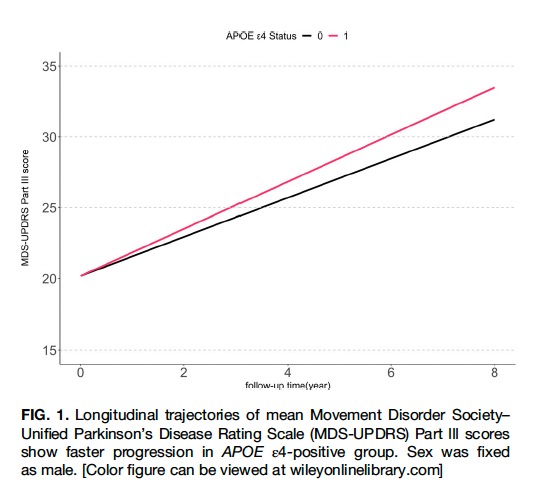
在帕金森病进展标志物计划中,他们从384名帕金森病患者中获得了纵向数据,这些患者分为APOE ε4携带者(n = 85)和非携带者(n = 299)。参与者在平均78.9个月的随访期间每年接受一次运动评估。重复测量和线性混合模型被用来检验APOE ε4的影响。
他们发现:与非携带者相比,携带APOE ε4的PD患者的运动进展明显更快(β = 0.283,P = 0.026,95%置信区间:0.033-0.532)。
通过亚组分析,我们发现APOE ε4的影响仅在高淀粉样β负担的患者中显著(β = 0.761,P < 0.001,95%置信区间:0.0356-1.167)。
这个研究的重要意义在于发现了:APOE ε4可能与PD的快速运动进展有关。
原文出处:
Pu J, Jin C, Wang Z, et al. Apolipoprotein E Genotype Contributes to Motor Progression in Parkinson’s Disease. Mov Disord. Published online October 6, 2021:mds.28805. doi:10.1002/mds.28805
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#Disord#
72
#Dis#
96
#运动障碍#
87
#APOE#
131
临床研究可以观察
107
好好学习
108
学习了,谢谢分享
89
好好学习好好学习
0