Gastroenterology:mTORC1/2聚集在Arp2/3复合体上促进腺泡→导管化生→早期胰腺癌转化进展
2021-01-05 MedSci原创 MedSci原创
致癌基因Kras通过以肌动蛋白为基础的形态发生过程-腺泡-导管化生(ADM)诱导胰腺腺泡细胞的肿瘤转化,并导致胰腺导管腺癌(PDAC)。mTOR复合物1(mTORC1)和2(mTORC2)分别含有Rp
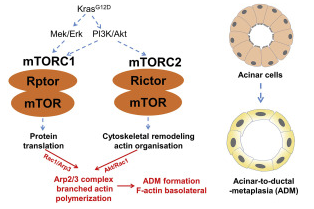
致癌基因Kras通过以肌动蛋白为基础的形态发生过程-腺泡-导管化生(ADM)诱导胰腺腺泡细胞的肿瘤转化,并导致胰腺导管腺癌(PDAC)。mTOR复合物1(mTORC1)和2(mTORC2)分别含有Rptor和Rictor,并在Kras下游被激活,从而促进PDAC的形成。然而,mTORC1和mTORC2是否以及如何影响ADM,以及介导这种肌动蛋白重排的肌动蛋白核因子的身份仍不清楚。
采用炎症加速Kras诱导的小鼠早期胰腺癌模型。在腺泡细胞中,条件性消融Rptor、Rictor或Arpc4(肌动蛋白相关蛋白2/3复合体4)以激活mTORC1、mTORC2和肌动蛋白相关蛋白(Arp)2/3复合体的功能。
mTORC1和mTORC2协同促进KrasG12D诱导的ADM和胰腺癌发生
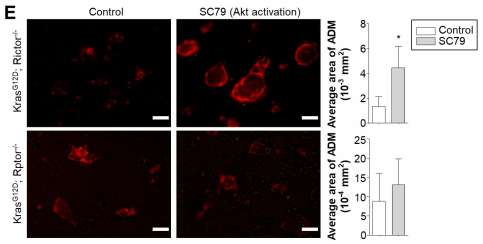
结果发现,mTORC1和mTORC2在人和小鼠的ADM病变中被显著激活,并在小鼠体内和体外协同促进Kras驱动的ADM。它们利用Arp2/3复合体作为共同的下游效应器来诱导肌动蛋白细胞骨架重塑,从而导致ADM。此外,mTORC1调控Rac1(Rac家族小GTPase 1)和Arp2/3-复合体亚基Arp3的翻译,而mTORC2通过促进Akt/Rac1信号通路激活Arp2/3复合体。
mTORC2通过Akt/Rac1信号轴激活Arp2/3复合物
与上述结果一致,消融Arp2/3复合体基因可以在体内阻止Kras驱动的ADM。在腺泡细胞中,Arp2/3复合体及其肌动蛋白核活性介导了基底外侧肌动蛋白皮质的形成,这是ADM和癌前转化所必需的。
本研究表明,mTORC1和mTORC2通过促进Arp2/3复合体功能,在ADM和早期胰腺癌发生中起到双重但非冗余的调节作用。因此,Arp2/3复合体作为mTORC1和mTORC2的共同效应器填补了致癌信号和PDAC启动的肌动蛋白动力学之间的空白。
原始出处:
Zhao Yamin,Schoeps Benjamin,Yao Dianbo et al. mTORC1 and mTORC2 converge on the Arp2/3 complex to promote Kras-induced acinar-to-ductal metaplasia and early pancreatic carcinogenesis.[J] .Gastroenterology, 2020, 10.1053/j.gastro.2020.12.061.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Gastroenterol#
64
#AST#
78
#GAS#
67
#复合体#
78
#mTORC1#
51
#Gastroenterology#
66
#肿瘤#胰腺癌
139