Science:模拟老年痴呆的分子机制居然能治癌
2016-11-14 MedSci MedSci原创
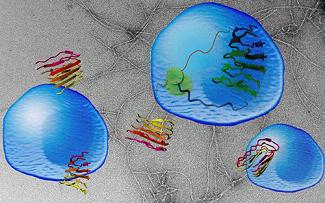
比利时VIB鲁汶大学Switch实验室在11月11日Science上揭示了一个新设计的分子,能通过淀粉样蛋白的形成机制有效抑制癌症的发生。这项工作表明:根据淀粉样蛋白的结构可以合理地开发一种新的生物分子,能够对抗各种各样的疾病。经过十多年的研究,比利时VIB鲁汶大学Switch实验室揭示了一个新设计的分子,能通过淀粉样蛋白的形成机制有效抑制癌症的发生。这项工作表明:根据淀粉样蛋白的结构可以合理地开
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#治癌#
55
意外发现
131
#SCIE#
64
很好,不错,以后会多学习
117
不错的探索
115