ASCO2017:黑色素瘤检查点抑制剂经验告诉我们关于其他癌症的免疫治疗?
2017-06-06 MedSci medicalxpress
自从2002年在黑素瘤患者中首次测试检查点抑制剂ipilimumab和tremelimumab之后,癌症免疫治疗领域的试验激增,增加了数百起新的试验,在肿瘤疗法领域的发展也迅猛增加。Ipilimumab,nivolumab和pembrolizumab已经成为治疗转移性黑色素瘤的主要治疗手段,但是更重要的临床发展是美国食品和药物管理局(FDA)批准三种不同的抗PD-1 / -PD-L1药物在非小
自从2002年在黑素瘤患者中首次测试检查点抑制剂ipilimumab和tremelimumab之后,癌症免疫治疗领域的试验激增,增加了数百起新的试验,在肿瘤疗法领域的发展也迅猛增加。Ipilimumab,nivolumab和pembrolizumab已经成为治疗转移性黑色素瘤的主要治疗手段,但是更重要的临床发展是美国食品和药物管理局(FDA)批准三种不同的抗PD-1 / -PD-L1药物在非小细胞肺癌,肾癌,头颈癌和膀胱癌,以及霍奇金淋巴瘤。获得用于不同类型肿瘤的审核不会太久,大量的联合试验正在进行,以优化检查点抑制剂的使用。黑色素瘤患者的经验教训无疑将有助于加速其他癌症检查点抑制的发展并可能提出治疗免疫耐药性癌症患者的新策略,如前列腺癌,胰腺癌和非微卫星不稳定性高结肠癌。
反应动力学
早期黑色素瘤检查点抑制剂的开发,其独特的反应动力学变得明显。响应的模式包括6到12个月的缓慢回归,随后发生混合反应,接着是回归后进展。尽管在多达10%的患者身上发现了这些不同寻常的模式,他们提出了一个问题,那就是在疾病恶化之后,需坚持治疗多久,或者在面对复杂的反应时是否继续治疗。这些问题引发了免疫反应使用标准或者是不受RECIST影响的标准的修改。没有临床或生物化学恶化的病人的疾病进展需要通过重复的短间隔扫描进行确认。对于这些患者,在宣布疾病进展之前,允许更大的耐受性以适应增加的肿瘤负荷。这些概念将需要应用于用检查点抑制治疗的其他组织上。
应答持续时间
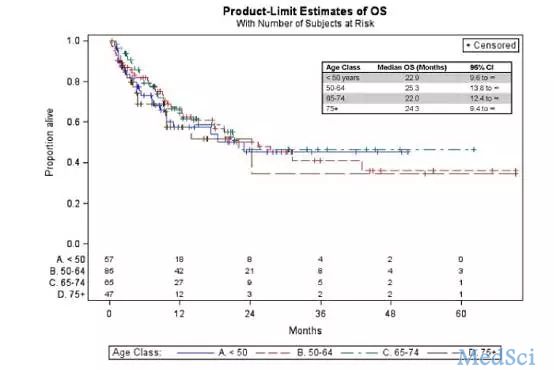
癌症免疫治疗领域的一个关键问题是治疗患者使用检查点抑制剂的治疗时间。黑色素瘤的早期试验允许治疗直到疾病进展;那么,2年是最大持续时间,有几份报告检查了对免疫检查点抑制剂有应答的患者在停止用药2到3年后的情况。在大多数情况下,完全应答的患者在停止治疗后可保持缓解。许多没有达到完全应答并且疾病进展的人能够对进一步的免疫治疗作出反应。对于获得部分缓解的人,已经观察到类似的数据。黑色素瘤存活的"尾巴曲线"的存在,现在还有其他癌症,表明许多检查点抑制作用的反应者可能会被治愈,或者至少具有长期的免于疾病进展的免疫力,并且不需要进行治疗。持续治疗时间不少于1年不超过2年似乎是合理的。
免疫相关毒性
用ipilimumab观察到的独特的副作用模式和使用PD-1 / PD-L1抑制剂对于那些没有使用这些药物的医生来说是一个挑战。针对这些与免疫相关的不良事件的成功管理已经建立了算法,这是与检查点抑制的作用模式相关的并且与耐受性破坏直接相关的机制。在几乎所有使用这些药物的癌症中,将根据所使用的组合疗法和每种癌症的独特病理生理学来观察特定的副作用模式。有一些数据表明,与免疫相关的不良事件的出现与更好的结果相关联,但它可能是免疫调节剂如类固醇和抗肿瘤坏死因子抗体(infliximab)的需要,这类免疫调节剂实际上是与利益相关的。在肺癌患者中,使用PD-1阻滞剂或PD-1阻滞剂与CTLA阻滞剂联用出现肺炎的几率大于黑色素瘤患者。并且白癜风和其他皮肤效应在黑素瘤中可能比其他癌症更常见。因此临床医生必须有一个低的阈值来排除有非特异性疲劳症状的内分泌疾病,偶尔使用短期类固醇方案来治疗可能对那些伴有2级副作用的患者有用,临床医生必须意识到3至4级免疫相关副作用需要更长期的类固醇治疗。
生物标记物
在检查点抑制剂领域最令人头疼的问题是,是否可以定义生物标记来预测使用这些药物的回归模型,从而使临床医师能够选择最有可能对他们作出反应的病人。在患有黑素瘤或非小细胞肺癌的患者中,有很多研究表明肿瘤可分为三类:那些被T细胞浸润并趋向于具有肿瘤基因表达的"炎性"或"热"特征,在组织学上没有任何T细胞或炎症浸润的肿瘤,并且具有非发炎或"冷"特征,在肿瘤周边但不具有T细胞和其他免疫细胞的肿瘤。"热"肿瘤是最可能对PD-1 / PD-L1阻断作用的肿瘤,并且已被引发除了具有高水平PD-1的T细胞。许多研究已经评估了PD-L1肿瘤和/或免疫细胞免疫组织化学染色的作用及其与PD-1 / PD-L1阻断结局的关系。尽管大多数研究认为膜质肿瘤PD-L1水平越高PD-1 / PD-L1阻断效果越好,很明显,肿瘤染色PD-L1阴性的患者仍然可以从检查点抑制中获益。选择这类患者进行此类治疗,否定了PD-L1的效用,因为它无法确定哪些病人不应该被治疗。
表达PD-1和/或CTLA-4的肿瘤浸润性CD8 + T细胞的数量似乎是检查点抑制成功的关键指标。PD-1和CTLA-4阻断均可增加浸润性T细胞。
"聚焦"的T细胞受体谱与PD-1 / PD-L1阻断的良好结果相关,而与CTLA-4抗体的益处相关的T细胞受体谱更多样化的。T细胞谱系反映了宿主对癌症的免疫反应,但是肿瘤本身是检查点抑制成功的关键决定因素,因为增加的非同义变体或肿瘤突变和检查点抑制的结果之间存在关系。新抗原或可以被T细胞识别为抗原的突变蛋白质的数量与检查点抑制剂的结果密切相关。
肿瘤微环境的性质也在抵抗或对检查点抑制的敏感性方面起重要作用。反映一系列干扰素-γ的肿瘤基因表达特征--可诱导的基因可能定义为"炎症性"发炎的肿瘤,并且在多个研究中具有检测点抑制作用的良好结果。它的丧失与对ipilimumab治疗的耐药性有关。黑色素瘤是II类的主要组织相容性复合体,对PD- 1 /PD- L1的阻滞有积极反应,并可与之分享干扰素-γ响应特征。相反,耐药性肿瘤显示出转录特征(称为IPRES或先天性抗PD-1抗体),这与增加对上皮-间质过渡、细胞粘附、细胞外基质重构、血管生成和伤口愈合的调控的基因表达有关。
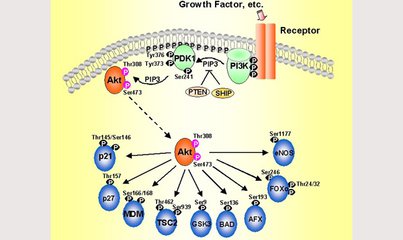
在黑色素瘤中常见的PTEN基因的缺失,对抑制肿瘤免疫具有抑制作用,并导致一个"冷"肿瘤,具有高水平的免疫抑制细胞因子,具有稀疏和非活性T细胞。WNT /β-连环蛋白信号通路的肿瘤活化与T细胞基因表达特征的缺失之间也存在关联,这导致了浸润性树突细胞和"冷"肿瘤微环境的缺陷。这可以通过使用STING激动剂来克服,其可以增加干扰素-γ途径基因的表达。PD-1阻断的大型临床试验中宿主生物标志物的临床检查显示,嗜中性粒细胞与淋巴细胞比例,基线乳酸脱氢酶和嗜酸性粒细胞数量与检查点阻滞的结果相关,尽管这些标记物都不能准确地定义哪些患者对治疗无效。
在表现出对检查点抑制的基线抵抗或在初始反应后对治疗产生适应性的抵抗的肿瘤中,诱导肿瘤JAK1和JAK2基因突变或β-2微球蛋白缺失可能是负责任的,导致T细胞免疫受损,无法检测肿瘤抗原。
毫无疑问,这将成为许多不同肿瘤类型的检测点蛋白质抑制的先天和适应性抗性的常见途径。对这些药物的成功预测将需要合并肿瘤细胞的内在和宿主T细胞特异性决定因素的混合生物标志物。
原文出处:
此文系梅斯医学(MedSci)原创编译整理,转载须授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#ASC#
112
#抑制剂#
73
#色素#
78
#黑色素#
81
#黑色素#
103
学习了,值得分享!
132
学习,谢谢分享
108
这个可以仔细研究一下
113