
英国每年有超过12万人经历脚踝骨折。到2030年,脚踝骨折预计将增加三倍。受影响的成年人长时间无法从事通常的体育活动。对个人的质量影响是巨大的,影响家庭和社会生活、睡眠、独立感和心理健康。传统上,骨折后脚踝被固定在僵硬的石膏中几周,这允许骨头愈合,但可能导致关节僵硬和肌肉无力。另一种选择是可拆卸的支架,可以摘下以允许早期活动。使用可拆卸支具可以防止僵硬固定的后果,并有助于加速恢复。这两种方法在英国都是常规使用的。Cochran认为,功能性支撑可以减少活动限制和疼痛,改善踝关节运动。然而,这些潜在的优势需要与不良事件发生率的增加相平衡。
鉴于踝关节骨折数量的增加和个人和社会的巨大成本,Rebecca Kearney等比较了可摘支具和石膏在功能、生活质量和并发症方面对成人踝关节骨折的影响。

该研究评价了成人踝关节骨折石膏固定与可摘支具固定治疗的功能、生活质量、资源利用和并发症。
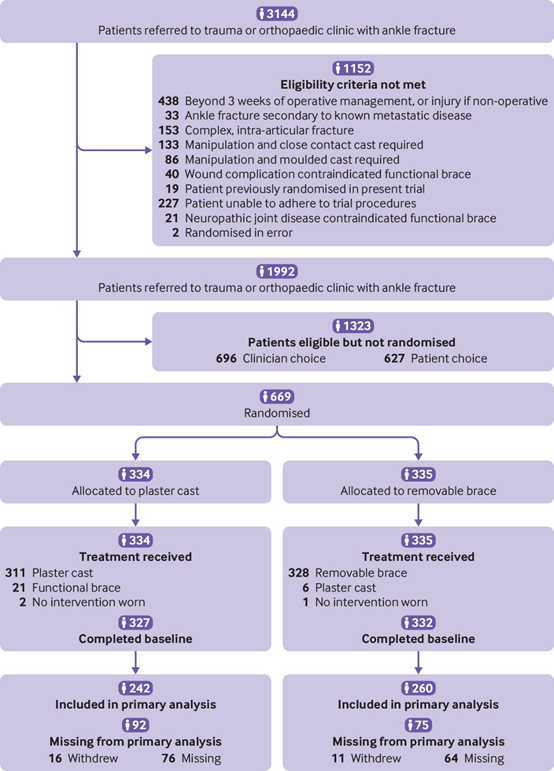
该团队在英国国家卫生服务中心的20个创伤科招募了669名年龄在18岁及以上的急性踝关节骨折适合石膏固定的成年人:334名被随机分为石膏组和335名可拆卸支具。对膝下石膏进行干预,并在去除石膏时开始踝关节活动范围的训练。安装了可拆卸支具,并立即开始踝关节范围的运动训练。主要观察指标为16周时Olerud Molander踝关节评分,按治疗意向分析。次要结果为6、10和16周时的曼彻斯特-牛津足问卷、残疾评定指数、生活质量和并发症。
两组的Olerud Molander踝关节评分(OMAS)
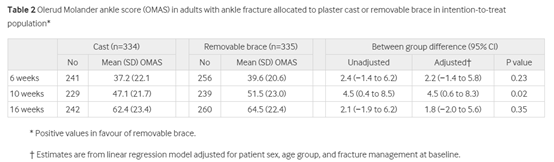
受试者平均年龄46岁(标准差17岁),女性381人(57%)。502名(75%)参与者完成了研究。16周时,石膏组和可拆卸支架组的Olerud Molander踝关节评分无统计学差异(Favors支架:1.8,95%置信区间)−2.0至5.6)。在其他时间点的Olerud Molander踝关节评分、二次未校正分析、推断分析或按方案分析中均未发现临床显著性差异。
这项随机对照试验发现,在踝关节骨折的成人16周时,石膏和可拆卸固定角支具在踝关节功能方面没有显著差异。95%置信区间的上限有效地排除了一种干预优于另一种干预的任何可能性。在二级时间点的Olerud Molander踝关节评分或曼彻斯特-牛津足部问卷的二级结局指标、残疾等级指数、生活质量和并发症方面没有发现临床相关差异。两种干预措施在严重并发症的安全性方面没有统计学上的显著差异。活动支具组出现的并发症较多,尤其是伤口破裂(7 v 15),伤口感染(10 v 19)和需要进一步手术(4 v 8)。
在成人踝关节骨折患者中,传统石膏固定并不优于功能性支具。16周时,试验组间Olerud-Molander踝关节评分无统计学差异。这项试验提供了强有力的证据,证明成人踝关节骨折的传统石膏固定和可拆卸支具在统计学上没有显著差异。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













继续关注➕
78
学习啦
74
#踝关节骨折#
105
#踝关节#
68
学习了
81
学习
70