腰椎间盘突出练倒走得不偿失
2017-09-18 郭仲华 主任医师 宁夏中医研究院骨科 中国中医药报
小张今年30岁,诊断为腰椎间盘突出症2个月,经过中医综合治疗,疼痛减轻,病情好转。几天前,他听邻居说练倒走可以治腰椎间盘突出症,便尝试倒着走路,谁料,刚走一段路一不小心却被井盖绊倒,腰痛顿时加重许多,走路更困难,医生建议住院治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





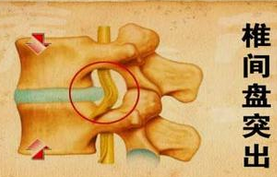








#椎间盘突出#
62
#腰椎#
93
#腰椎间盘#
68
学习了学习了学习了学习了学习了学习了学习了学习了学习了
141