Lancet:托珠单抗可明显改善住院治疗的合并低氧和系统性炎症的新冠肺炎患者的预后
2021-05-04 Nebula MedSci原创
对于住院治疗的伴有低氧和系统性炎症的新冠肺炎患者,托珠单抗治疗可提高其存活率和其他临床预后
大部分新冠肺炎病毒(SARS-CoV-2)感染者无明显症状或只表现出轻度的异常。但是,相当一部分感染者会发展成需要住院治疗的呼吸道疾病,甚至会进展成需要通气支持的严重呼吸衰竭。

本研究旨在评估住院治疗的伴有缺氧和全身性炎症的新冠肺炎(COVID-19)患者采用托珠单抗(tocilizumab)治疗的效果。
这是一项在英国开展的随机、对照、开放标签的平台试验,纳入了低氧(无吸氧时氧饱和度<92%或需要氧疗)、系统性炎症(C反应蛋白≥75 mg/L)的COVID-19患者,随机(1:1)分至两组,只接受标准治疗或标准治疗联合托珠单抗(400-800 mg)治疗。主要终点是28天时的死亡率。
2020年4月23日-2021年1月24日,RECOVERY试验招募的21550位患者中有4116位成年患者被纳入托珠单抗的评估,包括3385位(82%)接受了系统性皮质类固醇治疗的患者。
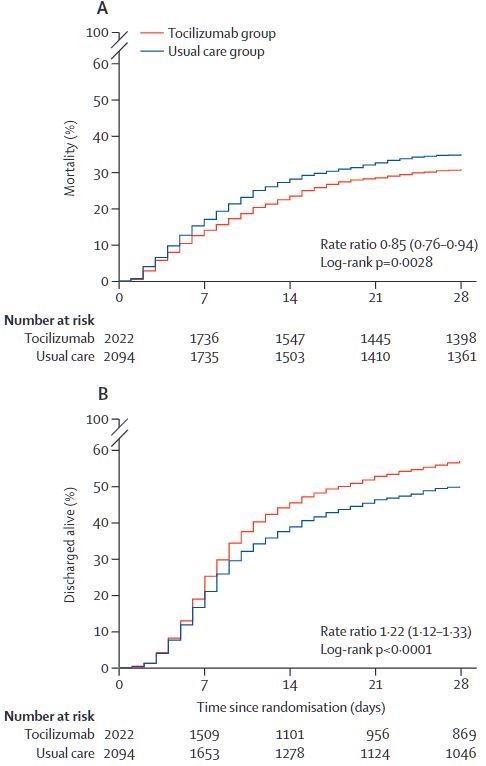
两组28天内的死亡率和出院率
总体上,2022位患者被分至托珠单抗组,2094位被分至常规治疗组。在28天内,托珠单抗组和常规治疗组分别有621位(31%)和729位(35%)患者死亡(发生率比 0.85,95% CI 0.76-0.94)。在所有预先指定的患者亚组分析中均观察到了一致的结果,包括那些接受全身性皮质类固醇激素治疗的患者。
托珠单抗组的患者更可能在29天内顺利出院(57% vs 50%,发生率比 1.22, 95% CI 1.12-1.33,p<0.0001)。在基线时未接受有创机械通气的患者中,接受托珠单抗治疗的患者不太可能达到有创机械通气或死亡的综合终点(35% vs 42%,发生率比 0.84, 95% CI 0.77-0.92,p<0.0001)。
综上所述,对于住院治疗的伴有低氧和系统性炎症的新冠肺炎患者,托珠单抗治疗可提高其存活率和其他临床预后,这些治疗益处且不受是否采用呼吸支持和皮质类固醇激素治疗的影响。
原始出处:
RECOVERY Collaborative Group. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. The Lancet. May 01, 2021. https://doi.org/10.1016/S0140-6736(21)00676-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#系统性#
72
#Lancet#
54
新冠肺炎,疫情何时才能消失
89
顶刊就是不一样,质量很高,内容精彩!学到很多
88
感兴趣
87
学习了,涨知识了!
73