Front Oncol:新辅助化疗(NAC)对比直接手术治疗局部进展期胃癌合并浆膜侵袭(cT4NxM0)患者的疗效
2021-12-14 yd2015 MedSci原创
研究表明, NAC可进一步改善LAGC (cT4NxM0)患者预后,预防复发,且安全可行,不增加围手术期手术风险。
对于局部进展期胃癌合并浆膜侵袭(cT4NxM0), D2胃切除术后+辅助化疗(AC)是亚洲人群的标准治疗方法。但欧美国家多建议围手术期化疗(PCT)联合D2胃切除术。作为PCT的一部分,新辅助化疗(NAC)的价值尚不明确。来自上海交通大学附属瑞金医院的团队开展了相关研究,评估NAC是否能进一步改善这些患者的生存和其他结果。相关结果发表在Frontiers in Oncology杂志上。

对cT4NxM0胃癌行D2胃切除术的患者进行分析。根据是否接受NAC分为新辅助化疗组(NAC)和直接手术组(S)。倾向评分匹配(1:1)后,分析两组患者的生存率和围手术期预后。
2013年1月至2018年12月,共有902例患者纳入研究。在902例患者中,375例(41.57%)患者死于胃癌,455例(50.44%)患者在随访最后一天出现复发。随访期间共有51例(5.65%)患者失联。在所有符合条件的患者中,285例(31.60%)患者接受NAC, 617例(68.40%)患者接受D2胃切除术后单独AC。NAC组3种肿瘤标志物(CA125、CA724、CEA)均显著高于S组(P<0.01)。临床N分期方面,NAC组N0-1期61例(21.40%),N2期139例(48.77%),N3期85例(29.82%)。S组N0-1期343例(55.59%),N2期227例(36.79%),N3期47例(7.62%)。
PSM后两组各有221例患者,其中男性331例,女性111例,男女比例为2.98:1。诊断时的中位年龄为62.50岁(范围:21-80岁)。NAC组分别有148例(66.97%)和73例(33.03%)患者达到PR和SD。20例患者获得TRG 0级。NAC组中,142例患者接受EOX治疗,59例接受SOX治疗,4例接受XELOX治疗,16例接受FLOT治疗。
总体人群的中位总生存期(OS)为75.10个月,中位无病生存期(DFS)为43.67个月。NAC组和S组患者的中位OS分别为未达到和29.80个月(P<0.0001, HR 0.34, 95% CI 0.25-0.46)。NAC组患者1年、3年、5年OS率分别为93.59%、78.82%、72.29%。S组患者1年、3年、5年OS率分别为83.71%、45.90%、36.22%。此外,NAC组和S组患者的中位DFS分别为未达到和为22.60个月(P<0.0001, HR 0.44, 95% CI 0.33 - 0.58)。NAC组患者1年、3年、5年DFS率分别为82.53%、69.74%、58.53%。S组患者1年、3年、5年DFS率分别为70.44%、39.86%、30.87%。
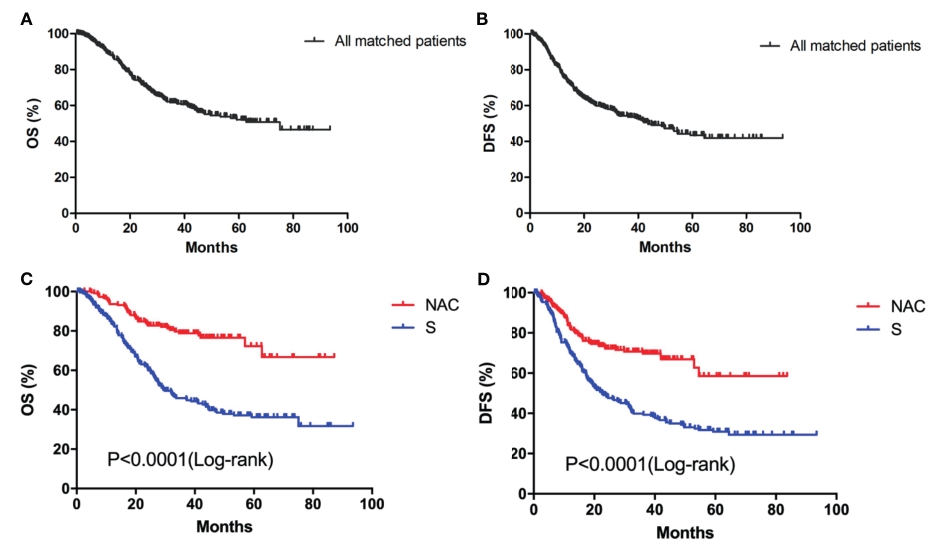
总体人群以及两组的OS和DFS
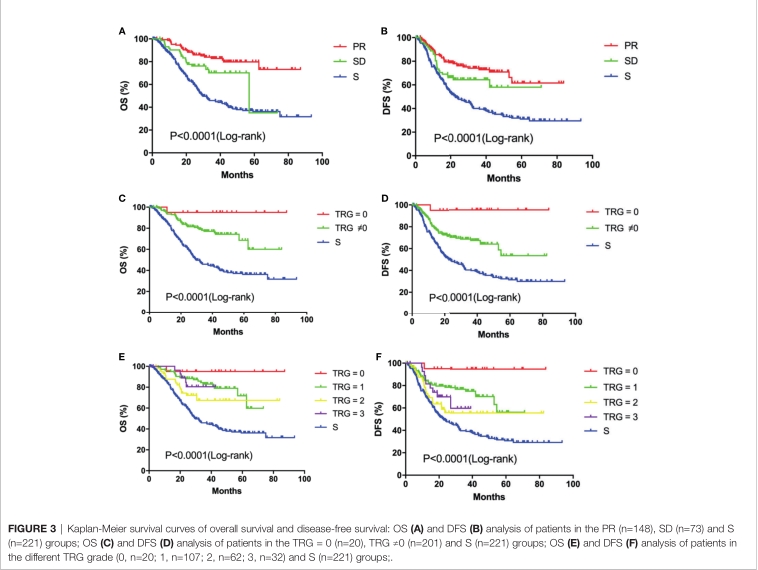
PR组和SD组患者的中位OS分别为未达到和56.97个月(P<0.05)。PR组患者1年、3年、5年OS率分别为95.21%、82.81%、79.82%。SD组患者1年、3年、5年OS率分别为90.28%、70.19%、35.09%。PR和SD患者的中位DFS均未达到,差异无统计学意义(P=0.07)。PR组患者1年、3年、5年DFS发生率分别为85.66%、72.78%、61.45%。SD组患者1年、3年和5年DFS分别为76.12%、64.27%和57.84%。NAC组20例(9.05%)患者为TRG 0级。TRG=0组和非TRG=0组的OS (P<0.05)和DFS (P<0.05) 有明显差异。TRG=0组患者1年、3年、5年OS和DFS均为95.00%。非TRG=0组患者1年、3年、5年OS率分别为93.45%、77.02%、68.57%。1年、3年和5年DFS率分别为81.27%、66.98%和53.03%。

PR、SD以及不同TRG的OS和DFS
PR组和SD组的OS和DFS率均显著高于S组(<0.0001)。不同TRG分级的OS和DFS率均显著高于S组(P<0.0001)。
不同亚组与手术(S)的OS和DFS对比
在NAC组和S组,分别有208例(94.12%)和197例(89.14%)患者行R0切除术。NAC组10例(4.52%)患者行R1切除术,3例(1.36%)患者行R2切除术。S组13例(5.88%)行R1切除术,11例(4.98%)行R2切除术。NAC组和S组中位淋巴结切除数目分别为34和38。两组患者手术根治程度、清扫淋巴结数量差异无统计学意义(P=0.07、P=0.124)。两组术后住院时间(P<0.001)和并发症(P=0.037)差异有统计学意义。

围手术期结果
综上,研究表明, NAC可进一步改善LAGC (cT4NxM0)患者预后,预防复发,且安全可行,不增加围手术期手术风险。
原始出处:
Xu W, Wang L, Yan C, He C, Lu S, Ni Z, Hua Z, Zhu Z, Sah BK, Yang Z, Zheng Y, Feng R, Li C, Yao X, Chen M, Liu W, Yan M and Zhu Z (2021) Neoadjuvant Chemotherapy Versus Direct Surgery for Locally Advanced Gastric Cancer With Serosal Invasion (cT4NxM0): A Propensity Score-Matched Analysis. Front. Oncol. 11:718556. doi: 10.3389/fonc.2021.718556
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#进展期#
145
#Oncol#
0
#新辅助#
94
受教了
86
#手术治疗#
98
#局部#
84