CHEST:美国慢性血栓栓塞性肺动脉高压注册:治疗首选肺动脉内膜切除术!
2021-11-10 刘少飞 MedSci原创
慢性血栓栓塞性肺动脉高压(CTEPH)最先进的治疗方法是肺动脉内膜切除术。 加州大学圣地亚哥分校小组由Kenneth Miles Moser教授创立,他培养了一支庞大的团队,影响着全球CTEPH医生。

慢性血栓栓塞性肺动脉高压(CTEPH)是一种罕见的阻塞性肺血管疾病,起源于有症状或无症状的肺栓塞。 CTEPH 最先进的治疗方法是肺动脉内膜切除术 (PEA),它是用先进的手术技术打开阻塞的肺动脉分支。 CTEPH 的机械治疗,如 PEA、球囊肺血管成形术(一种专为那些没有被选为手术候选人的经皮技术)和血管扩张药物的药物治疗在改善血流动力学、临床状态、右心室功能、和 CTEPH 患者的生存率。
在本期 CHEST 中,Kerr 等人报道了美国 CTEPH 患者的当代注册登记特征和 1 年随访。总体而言,美国 CTEPH Registry 是由加州大学圣地亚哥分校 (UCSD) 小组所负责的,该小组自 60 年代末以来一直是 PEA 的先锋。加州大学圣地亚哥分校小组由肯尼斯·迈尔斯·莫泽 (Kenneth Miles Moser) 创立,他培养了一支庞大的团队,从那时起,该团队将 CTEPH 技能传授给了全球几代 CTEPH 医生。
该研究报告了来自美国 CTEPH 注册中心的 30 个中心的 6 个月内诊断出的 750 名患者,并描述了手术和未手术受试者之间基线特征和 1 年结果的差异。正如预期的那样,数据表明可手术和不可手术的患者代表不同的疾病状况。可操作性评估正在筛选出一个特殊的 CTEPH 患者亚群,这些患者比不能手术的患者更年轻,更可能肥胖,有 DVT 病史,携带非 O 型血型或血栓形成倾向,并且不太可能有慢性阻塞性肺病或癌症病史。作者的主要发现是,接受 PEA 的患者预后最好,美国专家中心的 30 天死亡率为 3.9%,纽约心脏协会功能分级 1 或 2 的 1 年死亡率为 82.9%。
该报告很值得关注,因为该数据库反映了医疗和手术方法的演变,包括 riociguat 和皮下曲前列环素的市场批准以及自欧洲 CTEPH Registry 上次发表关于该主题的研究以及2011年球囊肺血管成形术的改进(表)。另一个优势是注册登记由两名影像评审员监督,这保证了以适当的严谨和技术实现 CTEPH 诊断。然而,从该数据收集与欧洲和中国前瞻性登记处的比较中可以看出(表),人群似乎偏向于手术候选人。
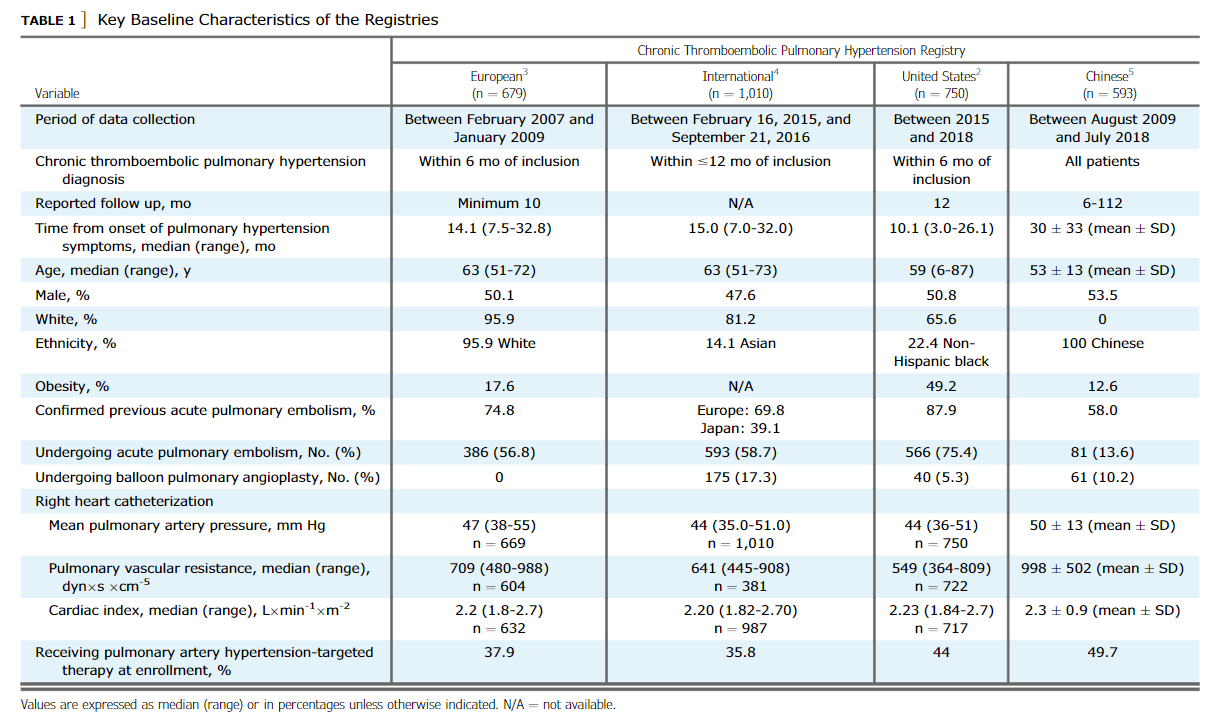
此外,白人和亚洲 CTEPH 人群之间存在显着差异,在性别(亚洲 CTEPH 女性患者较多)、BMI(美国肥胖较多)和球囊肺血管成形术频率(在美国总体上仍然较低) )。上表是当代前瞻性收集数据的分析,其中包括用于比较的 2011 年欧洲 CTEPH 注册表。数据将随时间变化,因为来自俄罗斯、日本、和中东人群的 CTEPH 人群将出现在文献中。此时此刻,来自美国的数据明显带有 PEA 的阴影,这促进了一种治疗策略,该策略已将数千名患者的生活从严重的右心衰竭转变为接近正常,但目前面临着挑战经皮球囊肺血管成形术。
文章出处:
Lang IM. Results From the United States Chronic Thromboembolic Pulmonary Hypertension Registry: Pulmonary Endarterectomy First! Chest. 2021 Nov;160(5):1599-1601. doi: 10.1016/j.chest.2021.07.004. PMID: 34743844.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#切除术#
81
#Chest#
105
#内膜#
75
#动脉高压#
83
#EST#
73
#注册#
127