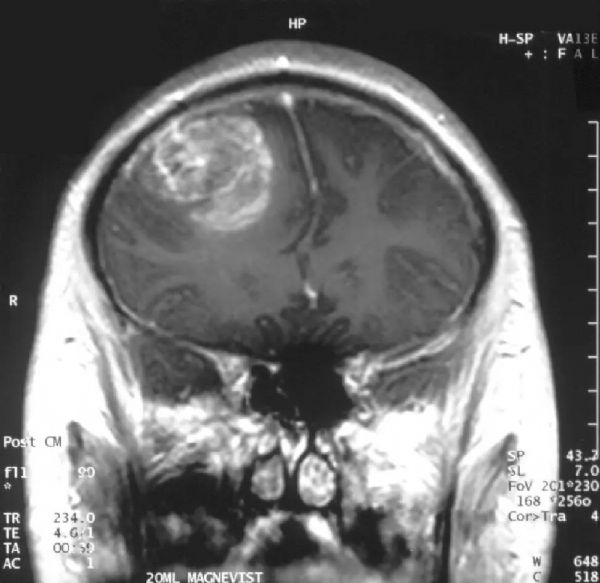
Nature子刊:华人学者千里挑一,找到脑瘤致命基因突变
2017-08-15 佚名 药明康德
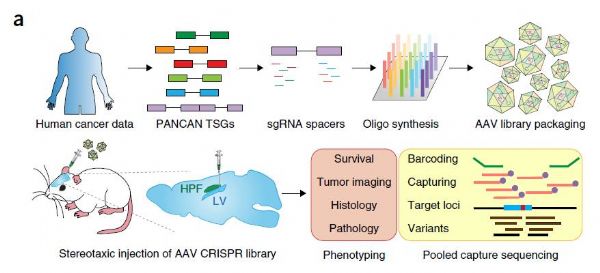
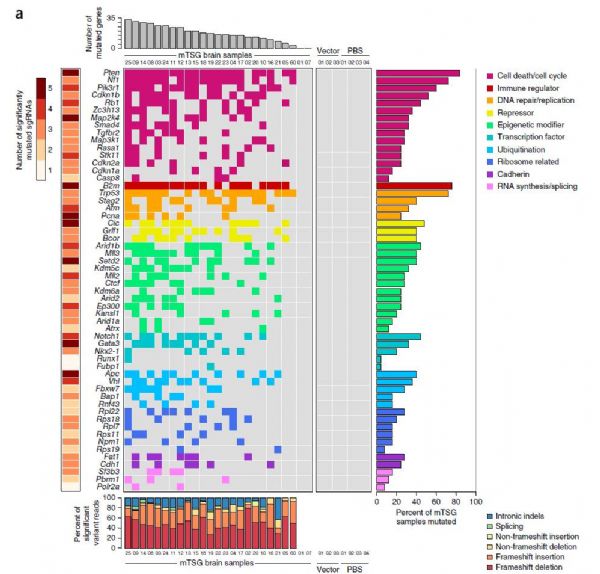
随着CRISPR基因编辑技术的不断成熟,越来越多奋斗在前沿的科学家们开始探索它的无限应用潜力。上周,我们报道了两则相关的新闻:张锋教授协助的一项研究使用CRISPR技术,寻找到了一个与癌症免疫疗法相关的基因;杨璐菡博士的团队则使用该技术,让猪体内的内源性病毒序列失活,解决了异种器官移植的一大难题。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
98
#致命基因突变#
106
#脑瘤#
64
#华人#
98
#华人学者#
81