AGING CELL:心磷脂重塑联系线粒体功能障碍与帕金森病
2019-03-10 海北 MedSci原创
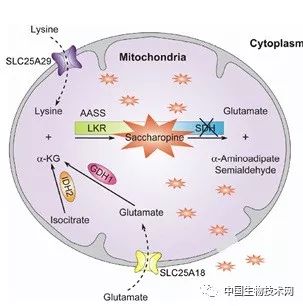
心磷脂(CL)是线粒体特征性磷脂,其是膜结构,呼吸,动力学和线粒体自噬所必需的。活性氧对CL的氧化损伤与帕金森病(PD)的发病机制有关,但至今为止,其根本原因仍然难以捉摸。
心磷脂(CL)是线粒体特征性磷脂,其是膜结构,呼吸,动力学和线粒体自噬所必需的。活性氧对CL的氧化损伤与帕金森病(PD)的发病机制有关,但至今为止,其根本原因仍然难以捉摸。
最近的一项研究在1-甲基-4-苯基-1,2,4,6-四氢吡啶(MPTP)诱导的PD小鼠模型中研究了ALCAT1(一种催化CL在各种衰老相关疾病中的病理重塑的酰基转移酶)的作用。
研究人员发现,MPTP处理能够引起中脑的氧化应激,mtDNA突变和线粒体功能障碍。相反,ALCAT1基因的消除或ALCAT1的药理学抑制阻止了MPTP诱导的神经毒性,细胞凋亡和运动缺陷。ALCAT1缺陷还通过调节DRP1易位至线粒体来减轻线粒体功能障碍。此外,ALCAT1的药理学抑制通过促进Parkin向功能失调的线粒体的募集,显着改善了线粒体自噬。
最后,ALCAT1的表达被MPTP和α-突触核蛋白病(PD的一个关键标志)上调,而ALCAT1缺陷阻止了α-突触核蛋白寡聚化和S-129磷酸化,这暗示了ALCAT1在PD小鼠模型的病因学中的关键作用。
总之,这些发现将ALCAT1鉴定为治疗PD的新型药物靶标。
原始出处:
Chengjie Song et al. Cardiolipin remodeling by ALCAT1 links mitochondrial dysfunction to Parkinson’s diseases. AGING CELL, 2019; doi: https://doi.org/10.1111/acel.12941
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
105
#线粒体功能#
127
#Cell#
69
#功能障碍#
0
#线粒体功能障碍#
136