ESC2018丨PFO封堵:复发性卒中风险降低的介入方法
2018-09-01 国际循环编辑部 国际循环
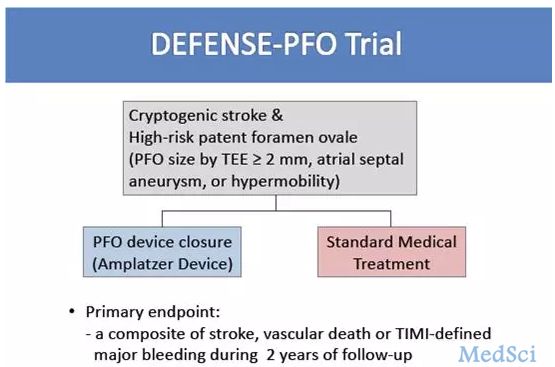
2018年欧洲心脏病学学会大会上,英国伦敦帝国理工学院哈默史密斯医院Iqbal Malik博士发表卵圆孔未闭(PFO)封堵可降低卒中复发风险的精彩报告,并指出ESC成员国每年大约有150万次卒中发病,美国每年有80万次卒中发病,其中,近1/3是隐源性卒中。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#复发性#
86
#PFO#
109
#ESC2018#
58
#风险降低#
105
#卒中风险#
55
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
67
中风是俗称,应该称为缺血性卒中吧
71